Abstract
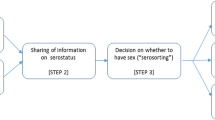
Seroadaptive behaviors have been widely described as preventive strategies among men who have sex with men (MSM) and other populations worldwide. However, causal links between intentions to adopt seroadaptive behaviors and subsequent behavior have not been established. We conducted a longitudinal study of 732 MSM in San Francisco to assess consistency and adherence to multiple seroadaptive behaviors, abstinence and condom use, whether prior intentions predict future seroadaptive behaviors and the likelihood that observed behavioral patterns are the result of chance. Pure serosorting (i.e., having only HIV-negative partners) among HIV-negative MSM and seropositioning (i.e., assuming the receptive position during unprotected anal sex) among HIV-positive MSM were more common, more successfully adhered to and more strongly associated with prior intentions than consistent condom use. Seroconcordant partnerships occurred significantly more often than expected by chance, reducing the prevalence of serodiscordant partnerships. Having no sex was intended by the fewest MSM, yet half of HIV-positive MSM who abstained from sex at baseline also did so at 12 month follow-up. Nonetheless, no preventive strategy was consistently used by more than one-third of MSM overall and none was adhered to by more than half from baseline to follow-up. The effectiveness of seroadaptive strategies should be improved and used as efficacy endpoints in trials of behavioral prevention interventions.

Similar content being viewed by others
References
Centers for Disease Control and Prevention. Consultation on serosorting practices. http://www.cdc.gov/hiv/topics/research/resources/other/serosorting.htm. Accessed 5 Nov 2010.
Le Talec J, Jablonski O. Seroadaptation instead of serosorting: a broader concept and a more precise process model. In: XVII International AIDS Conference, Mexico City, 2008, Abstract WEPE 0311.
van de Ven P, Kippax SC, Crawford JM, et al. In a minority of gay men, sexual risk practice indicates strategic positioning for perceived risk reduction rather than unbridled sex. AIDS Care. 2002;14:471–80.
Parsons JT, Schrimshaw EW, Wolitski RJ, et al. Sexual harm reduction practices of HIV-seropositive gay and bisexual men: serosorting, strategic positioning, and withdrawal before ejaculation. AIDS. 2005;19(Suppl. 1):S13–25.
Mao L, Crawford JM, Hospers HJ, Prestage GP, Grulich AE, Kippax SC. “Serosorting” in casual anal sex of HIV-negative gay men is noteworthy and is increasing in Sydney, Australia. AIDS. 2006;20:1204–6.
Truong HM, Kellogg T, Klausner JD, et al. Increases in sexually transmitted infections and sexual risk behaviour without a concurrent increase in HIV incidence among men who have sex with men in San Francisco: a suggestion of HIV serosorting? Sex Transm Infect. 2006;82:461–6.
Elford J, Bolding G, Sherr L, Hart G. No evidence of an increase in serosorting with casual partners among HIV-negative gay men in London, 1998–2005. AIDS. 2007;21:243–5.
Golden MR, Stekler J, Hughes JP, Wood RW. HIV serosorting in men who have sex with men: is it safe? J Acquir Immune Defic Syndr. 2008;49:212–8.
Velter A, Bouyssou-Michel A, Arnaud A, Semaille C. Do men who have sex with men use serosorting with casual partners in France? Results of a nationwide survey (ANRS-EN-Presse Gay 2004). Euro Surveill. 2009;14:pii19416.
Eaton LA, Kalichman SC, O’Connell DA, Karchner WD. A strategy for selecting sexual partners believed to pose little/no risks for HIV: serosorting and its implications for HIV transmission. AIDS Care. 2009;21:1279–88.
Zablotska IB, Imrie J, Prestage G, et al. Gay men’s current practice of HIV seroconcordant unprotected anal intercourse: serosorting or seroguessing? AIDS Care. 2009;21:501–10.
Liu C, Hu H, Goparaju L, et al. Sexual serosorting among women with or at risk of HIV infection. AIDS Behav. 2011;15:9–15.
Reniers G, Helleringer S. Serosorting and the evaluation of HIV testing and counseling in countries with generalized epidemics. AIDS Behav. 2011;15:1–8.
Snowden JM, Raymond HF, McFarland W. Prevalence of seroadaptive behaviors of men who have sex with men, San Francisco, 2004. Sex Transm Infect. 2009;85:469–76.
Snowden J, Raymond HF, McFarland W. Seroadaptive behaviors among men who have sex with men in San Francisco: The situation in 2008. Sex Transm Infect. 2011;87:162–4.
MacKellar D, Gallagher K, Finelayson T, Sanchez T, Lansky A, Sullivan PS. Surveillance of HIV risk and prevention behaviors of men who have sex with men-a national application of venue based, time-space sampling. Public Health Rep. 2007;122(Suppl. 1):S39–47.
Magnani R, Sabin K, Saidel T, Heckathorn D. Review of sampling hard-to-reach and hidden populations for HIV surveillance. AIDS. 2005;19(Suppl 1):S67–72.
McFarland W, Chen Y-H, Raymond HF, et al. HIV seroadaptation among individuals, within sexual dyads, and by sexual episodes, men who have sex with men, San Francisco, 2008. AIDS Care. 2011;23:261–8.
Vittinghoff E, Douglas J, Judson F, McKirnan D, MacQueen K, Buchbinder S. Per-contact risk of human immunodeficiency virus transmission between male sexual partners. Am J Epidemiol. 1999;150:306–11.
Page-Shafer K, Dilley J, McFarland W, et al. Risk of HIV infection attributable to oral sex among men who have sex with men and in the population of men who have sex with men. AIDS. 2002;16:2350–2.
Quinn TC, Wawer MJ, Sewankambo N, et al. Viral load and heterosexual transmission of human immunodeficiency virus type 1, Rakai Project Study Group. N Engl J Med. 2000;342:921–9.
Das M, Chu PL, Santos GM, et al. Decreases in community viral load are accompanied by reductions in new HIV infections in San Francisco. PLoS One. 2010;5:e11068.
Poudel KC, Poudel-Tandukar K, Yasuoka J, Jimba M. HIV superinfection: another reason to avoid serosorting practice. Lancet. 2007;370:23.
Bull SS, Lloyd L, Rietmeijer C, McFarlane M. Recruitment and retention of an online sample for an HIV prevention intervention targeting men who have sex with men: the Smart Sex Quest Project. AIDS Care. 2004;16:931–43.
Centers for Disease Control and Prevention. HIV prevalence, unrecognized infection, and HIV testing among men who have sex with men—five US cities, June 2004–April 2005. MMWR. 2005;54:597–601.
Centers for Disease Control and Prevention. Prevalence and awareness of HIV infection among men who have sex with men—21 cities, United States, 2008. MMWR. 2010;59:1201–7.
Pilcher CD, Tien HC, Eron JJ, et al. Brief but efficient: acute HIV infection and the sexual transmission of HIV. J Infect Disease. 2004;189:1785–92.
Pinkerton SD. Acute HIV infection increases the dangers of serosorting. Am J Prevent Med. 2008;35:184.
Centers for Disease Control and Prevention. Compendium of evidence-based HIV prevention interventions. http://www.cdc.gov/hiv/topics/research/prs/evidence-based-interventions.htm (2009). Accessed 6 Nov 2010.
Crepaz N, Lyles CM, Wolitski RJ, et al. Do prevention interventions reduce HIV risk behaviours among people living with HIV? A meta-analytic review of controlled trials. AIDS. 2006;20:143–57.
Morin S, Shade SB, Steward WT, et al. A behavioral intervention reduces HIV transmission risk by promoting sustained serosorting practices among HIV-infected men who have sex with men. J Acquir Immune Defic Syndr. 2008;49:544–51.
Kajubi P, Kamya MR, Kamya S, Chen S, McFarland W, Hearst N. Increasing condom use without reducing HIV risk: Results of a controlled, community trial in Uganda. J Acquir Immune Defic Syndr. 2005;40:77–82.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McFarland, W., Chen, YH., Nguyen, B. et al. Behavior, Intention or Chance? A Longitudinal Study of HIV Seroadaptive Behaviors, Abstinence and Condom Use. AIDS Behav 16, 121–131 (2012). https://doi.org/10.1007/s10461-011-9936-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-011-9936-8