Abstract
Chlamydia trachomatis is the most frequent cause for sexually transmitted diseases in European countries. The organism has an intracellular habitat with a very specific life cycle. A variety of diagnostic tests have been developed with different sensitivity and specificity. Interpretation of these tests can sometimes be difficult. Diseases caused by C. trachomatis in men comprise urethritis, prostatitis, epididymitis, infertility and reactive arthritis. Especially in prostatitis, the exact role of C. trachomatis is still under debate for the technical difficulties localizing the pathogen to the prostate. For treatment, only some antibiotics are effective because of the intracellular habitat of the pathogen. Prevention of infection comprises treatment and screening efforts.
Similar content being viewed by others
Introduction and taxonomy
Chlamydiae are metabolically deficient in their ability to synthesize ATP and thus require an exogenous source of this high-energy compound [2]. They are therefore obligate intracellularly growing bacteria. They are widespread throughout the world and infect both humans and animals. Currently, four species, Chlamydia pneumoniae, Chlamydia trachomatis, Chlamydia psittaci, and Chlamydia pecorum, belonging to the genus Chlamydia of the family Chlamydiaceae within the order Chlamydiales, are recognized [23]. C. pneumoniae and C. trachomatis are primarily human pathogens, C. psittaci and C. pecorum are primarily animal pathogens. C. pneumoniae has been recognized as a major cause of respiratory infections, C. trachomatis is a major cause of trachoma and sexually transmitted diseases in humans [23]. Because of its sequestered lifestyle, acquisition of exogenous DNA is considered to have played a limited part in the subsequent evolution of the species after the organisms moved into their intracellular niche and became environmentally and genetically isolated nearly a billion years ago [3]. Consequently, diversity in chlamydial genomes is mostly a result of nucleotide substitutions and gene loss. Over the course of evolutionary history, the accumulation of these differences has led to the present-day biovariants of C. trachomatis. Two biovariants exist within the human-specific strains, which together consist of 15 serovariants. The strains exhibit three distinct tissue tropisms upon infection. Among the trachoma biovar, serovars A, B, Ba and C are associated with ocular infection, and serovars D through K are associated with urogenital infection. Serovars L1, L2 and L3 compose the lymphogranuloma venereum (LGV) biovar and infect lymphatic tissue [3].
Epidemiology
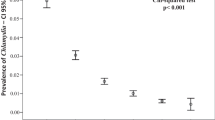
Genital C. trachomatis infections are among the most frequently encountered sexually transmitted diseases worldwide. It is currently estimated that about 4 million new chlamydial infections occur each year in the USA at an estimated annual cost exceeding 2.4 billion dollars [2]. Worldwide it is estimated that there are more than 50 million new cases of C. trachomatis infection annually. Although the major impact of disease is on the female genital tract, significant infections are also caused in men and newborns. Table 1 shows diseases caused by C. trachomatis serovars D–K in women, men and newborns. The prevalence in symptomatic women has been assessed in USA to be as much as 18%, in Scandinavia about 13%, whereas in asymptomatic women the prevalence was around 5% [9, 40]. Similarly, the prevalence in asymptomatic men in different studies using urine-based testing was around 5–7% [11, 38]. However, there exists a rather age-specific variation. Petersen et al. showed in a large surveillance study in Germany comprising 4381 persons (Fig. 1) aged 15–50 years, that women had the highest prevalence in the age group of 15–19 years with 7% followed by a rapid decline after the age of 25, and men had the highest prevalence in the age group of 20–24 years, also with a rapid decline after the age of 30 years [31]. There might however exist significant regional differences in prevalence due to different behaviour and health-care systems. In an ecological study comparing Uppsala county Sweden, and South East Thames region, England, the incidence of genital chlamydial infections and one of its consequences ectopic pregnancy was evaluated from 1988 to 1996 [19]. A significant decrease of chlamydial infections and ectopic pregnancies was found in Uppsala, whereas an increase over the years could be seen in SE Thames. The authors concluded that Chlamydia surveillance should be extended [19]. The biggest challenge to the control of chlamydial disease is that as many as 70–80% of women and up to 50% of men who are infected do not experience any symptoms, resulting in a large reservoir of unrecognized, infected individuals who are capable of transmitting the infection to sexual partners [2]. Immunity is thought to be type-specific and therefore only partially protective. Re-infections are common and probably complicating sequelae increase with multiple infections.
Prevalence of Chlamydia-trachomatis-infections amongst 4,381 asymptomatic persons in Germany [31]
Pathophysiology
The chlamydiae undergo a developmental cycle that is unique among prokaryotes. Following uptake, chlamydiae develop and grow within an intracellular vacuole, called an inclusion, that is distinct from all intracellular vacuolar compartments [26]. The inclusion membrane is devoid of host cell markers, but lipid markers traffic to the inclusion and suggest a functional interaction with the Golgi apparatus [36]. Within the inclusion, chlamydiae undergo a complex developmental cycle composed of functional and structurally distinct forms. The elementary body (EB) is infectious but is metabolically inactive and cannot replicate. This form differentiates upon infection into the non-infectious, but metabolically active, replicating reticulate body (RB) [26]. The EB and RB are phenotypically distinct. The EBs are spherical particles approximately 0.30 μm in diameter and possess a Gram-negative cell wall with an outer membrane composed of lipopolysaccharide (LPS), that is distinct from other bacteria and can be recognized as a genus-specific antigen [21]. At the surface the EBs harbour the outer membrane proteins that help for adhesion and invasion of the host cell, amongst an abundant protein termed the major outer membrane protein (MOMP, or OmpA), which is the major determinant for the serologic classification of chlamydial isolates. The MOMP of C. trachomatis allows the differentiation into 15 serovariants by monoclonal antisera. The EBs are osmotically resistant, and contain DNA that is exceedingly condensed into an electron-dense nucleoid. Within the first 2–6 h following internalization, EB begin differentiating into RB. The RBs are approximately 1 μm in diameter, are sensitive to osmotic lysis, and contain dispersed DNA. Over the next several hours, the RB increases in number and in size, until after 18–24 h, the number of RB is maximized. A vacuole can than contain up to 1,000 RBs and the large vacuole can occupy the majority of the volume of the host cell, without inducing apoptosis or fusing with the lysosomal granules [44]. After 24–48 h, increasing numbers of RBs begin differentiating back to EBs [26]. The infected cell ruptures approximately 48–72 h after infection, and the infectious EBs thus are released again onto the mucosal surface, but they might also become released through the basal membrane or into contiguous cells [44]. An intense and chronic inflammation is thus elicited and maintained. Whereas in the traditional view, the disease was regarded as an antigen-dependent delayed-type hypersensitivity or autoimmunity, it is now thought that the Chlamydia-infected non-immune mammalian cells produce pro-inflammatory chemokines, cytokines, growth factors and other cellular modulators. The inflammatory processes of chlamydial pathogenesis are thus elicited by infected host cells and are sufficient to account for chronic and intense inflammation and the promotion of cellular proliferation, tissue remodelling and scarring, the ultimate cause of the disease sequelae [43].
Diagnosis
Laboratory testing of C. trachomatis has traditionally consisted of cell culture of inocula prepared from urogenital specimens and later, the antigen and nucleic acid detection technologies were developed. The most recent nucleic acid amplification technologies have promoted widespread use of the detection of C. trachomatis. Specimen collection and transport is important to accuracy of diagnostic testing. As C. trachomatis is located intracellularly, it is generally important to harvest enough epithelial cells. For culture and antigen and nucleic acid detection of C. trachomatis, the most common site used to obtain specimens from women is the endocervix, which is sampled with a swab or brush [2]. It is also important to remove secretions and discharge from the cervix prior to sampling. The pooling of a urethral swab specimen increases the culture sensitivity by 23% [17]. In males, the preferred site of sampling is the anterior urethra. A dry swab is placed 3–4 cm into the urethra and rotated prior to removal. The subject should not have urinated within the previous hour. The likelihood of culturing is optimized if the specimens are refrigerated immediately after collection at 2–8°C and transported to the laboratory within 48 h. Molecular investigation techniques of C. trachomatis however have nowadays been accepted as the gold standard [32]. Additionally to the sites above, nucleic acid amplification tests also can detect C. trachomatis in urine samples. However, the specimens should be collected as first-catch specimen no less than 1–2 h of previous urination. Collection of vaginal introitus specimens has also been described to be sensitive for sampling in women, if nucleic acid amplification tests are applied [2]. The sampling for C. trachomatis in prostatitis traditionally comprised expressed prostatic secretions, urine after prostate massage and seminal plasma. Detection of C. trachomatis in prostatic secretions however has always been limited by the fact that potential contamination occurs by the passage of the specimens through the urethra. Therefore, efforts have been made to use prostatic tissue obtained under sterile conditions via biopsy, open operation or transurethral resection [52].
Culture
Culture detects only viable infectious chlamydial EBs. The sensitivity is maximal 70–85%, the specificity approaches 100%. The low sensitivity, the requirement for a stringent cold chain of transportation of specimens, costs, the high level of technical expertise necessary and the time required to obtain results, which ranks from 3 to 7 days, are significant disadvantages of this method. The advantage of culture is that additional investigations, such as genotyping or susceptibility testing can be performed [2].
Non-culture, non-nucleic acid amplification technologies
Non-culture, non-nucleic acid amplification technologies are based on direct visualization of the chlamydial organism by staining with fluorescein-labelled specific antibodies. The technologies comprise the direct cytologic examination (DFA) technique, the immunohistochemical detection of antigen (EIA), and the detection of hybridization to a DNA probe.
Direct cytologic examination (DFA)
In the DFA technique, monoclonal antibodies are directed either to the MOMP or the LPS antigens of Chlamydia. Antibodies to LPS react with all species of Chlamydia, antibodies to MOMP react specifically with C. trachomatis EB. The sensitivity of the DFA against MOMP of C. trachomatis is 80–90% and the specificity is 98–99% relative to the culture. The sensitivity however is lower with male urethral (<70%) than with endocervical specimens. The DFA test is rapidly performed within 30 min and does not require refrigeration of specimens during transport. However, the microscopic evaluation is laborious and requires experienced personnel [2].
Immunohistochemical detection of antigen (EIA)
The EIA diagnostic test is based on the immunochemical detection of LPS genus-specific antigen. In the direct EIA enzyme-labelled antibodies bind to LPS of EB and recognize all species of Chlamydia. In the indirect EIA, a primary anti-LPS antibody is used as the detector agent, followed by a secondary enzyme-linked antibody. Additionally a blocking test can be performed by repeating an initially positive EIA in the presence of monoclonal antibodies specific for chlamydial LPS. The initial positive signal is thus reduced, and if so the test is interpreted as a verification of the initial positive test result. The sensitivity of the EIA of male urethral C. trachomatis infection is 43–92% and the specificity is approximately 97%, with the blocking reagent >99% relative to the culture or the expanded culture (culture method plus another method added for definition of true positive). There are a variety of EIA tests commercially available with different sensitivity and specificity results. For example, the Chlamydiazyme EIA (Abbott Diagnostics, North Chicago, Illinois) has a sensitivity of 73% and a specificity of 97% for symptomatic male urine specimens. The Mikrotrak EIA (Behring) has a sensitivity of 97% and a specificity of 98% with male urethral specimens and a sensitivity of 82% and a specificity of 99% with male urine specimens [2].
Rapid tests (near-to-patient tests)
Rapid tests are performed in the physician’s offices and are based primarily on membrane capture or latex immunodiffusion. A variety of tests are available and are generally not well evaluated. Studies however showed that these tests are significantly less sensitive and less specific than the laboratory performed EIAs [2].
Nucleic acid detection methods
Nucleic acid detection methods consist of DNA-hybridization methods and DNA-amplification methods.
DNA-hybridization method
In the commercially available DNA-hybridization method for the detection of C. trachomatis (PACE 2, Gen-Probe, San Diego, CA, USA), a chemiluminescent DNA probe is employed. The probe hybridizes to a species-specific sequence of chlamydial 16S rRNA. Once the DNA–rRNA hybrid is formed, it is adsorbed onto a magnetic bead and the chemiluminescent response is detected quantitatively. The sensitivity of the DNA hybridization method of male urethral C. trachomatis infection is 85% and the specificity is approximately 98–99% relative to the culture or the expanded culture (culture method plus another method added for definition of true positive). The sensitivity relative to a DNA-amplification standard has been reported to be 77–93% [2].
DNA amplification methods
The most widely known of the DNA-amplification technologies is the polymerase chain reaction (PCR). The PCR test employs two synthetic oligonucleotide pimers with sequences that are complementary to the flanking regions of a specific DNA segment present in the target organism. After binding to the DNA template, the primers are extended through the activity of a thermostable DNA polymerase enzyme. Multiple cycles of denaturation, annealing, and extension of products result in logarithmic amplification of the DNA-target segment. The PCR products are deteceted by colorimetric capture-probe assay or by electrophoresis and staining with a DNA-intercalating fluorescent dye. There are several target gens for the PCR technology in C. trachomatis. In the Amplicor test (Roche diagnostics), the primers target a segment of the cryptic plasmid DNA present in C. trachomatis strains. The plasmid is present at seven to ten copies per genome; therefore the sensitivity of this test is very high. Amplicor PCR has been evaluated for both urogenital and urine specimens, sensitivity is 90% and specificity 99–100% relative to an expanded culture standard. Another target is the MOMP gene. The MOMP PCR is somewhat less sensitive, however the MOMP gene can be amplified almost in full length and the amplicon can be digested with restriction enzymes resulting in typical patterns representing different serovars. Therefore, this methodology can be used for epidemiological investigations without the need for culturing.
The polymerase can be inhibited by different substances in the specimen, such as nitrite, β-HCG, hemoglobin, and various salts, which changes the PCR results in about 5% [20]. Therefore, the ligase chain reaction (LCR) (Abbot Laboratories) was developed which also targets the C. trachomatis plasmid. In the LCR test, four synthetic oligonucleotide probes (two per DNA strand) anneal at the plasmid DNA. Each pair of probes hybridizes close together on the target template, with only a 1–2-nucleotide gap in between. Once the probes are annealed, the gap is filled by the DNA polymerase and closed by the ligase enzyme. The ligated probe pairs anneal to each other and, upon denaturation, form the template for successive reaction cycles, thus producing a logarithmic amplification of the target sequence. Inhibition of the probes occurs in about 2.5%. The sensitivity of urine specimens is 94%, the specificity is 99–100% relative to an expanded standard method [2]. In general, however the study data suggest that both PCR and LCR technologies will perform similarly for both urogenital and urine specimens. All nucleic acid amplification technologies detect nucleic acid targets and do not depend on the viability of the organism. This fact has to be kept in mind when analysing results of the tests.
A comparison of the relative limits of detection of the different technologies used described above, is shown in Fig. 2.
A comparison of the relative limits of detection of the different technologies used to diagnose C. trachomatis. The data are log numbers of chlamydial elementary bodies detected (after [2])
Serologic tests
Antibody-detecting serologic tests were developed for the diagnosis of C. trachomatis. Complement fixation (CF), microimmunofluorescence test (MIF), EIA, and p-ELISA. systemic serologic tests are generally not useful in the diagnosis of genital tract infections caused by C. trachomatis, perhaps except for LGV. This is because antibodies elicited by C. trachomatis are long-lived and a positive antibody test will not distinguish a previous infection from a current one [2].
Complement fixation test
The CF test detects the complement-fixing antibodies that recognize the genus-specific LPS antigen and is not specific for any one chlamydial species. It is the most sought after test for the diagnosis of LGV.
Microimmunofluorescence test
The MIF test detects species- and serovar-specific antibodies that probably react with species- and serovar-specific epitopes in chlamydial MOMP. The test is highly reliable in all the populations for the detection of a prior exposure to chlamydiae by the presence of IgG antibodies. The IgM antibodies are usually not present in patients with genital tract infections unless they represent the first exposure of the individual.
EIA test
The EIA test detects reactivity to genus-specific antigen, or LPS, of chlamydial elementary or reticulate bodies. The test is not specific for C. trachomatis.
p-ELISA test
Modern C. trachomatis peptide-ELISAs (p-ELISA) using a synthetic peptide from the immuno-dominant region of the MOMP seems to be able to discriminate C. trachomatis-specific antibodies in urethral secretions [39].
The high number of the diagnostic technologies described and the most different nature of these tests pose sometimes difficulties in interpreting the test results. The Centers for Disease Control have therefore set up guidelines for the diagnosis of infections with non-LGV strains of C. trachomatis [5, 6], that are shown in Table 2.
Urogenital diseases in men
Urogenital diseases in men caused by C. trachomatis comprise urethritis, prostatitis, epididymitis, infertility and reactive arthritis, which can extend to the full clinical picture of Reiter’s syndrome.
Urethritis
The urethritis is the initial infection with C. trachomatis in the male and can ascend from there to the contiguous urogenital organs. If the infection has been acquired together with a gonorrhoea and the antibiotic treatment has not eradicated the chlamydia, the infection is also called postgonococcal urethritis. Clinical presentation includes dysuria, pollakisuria and urethral pain without voiding. Urethral discharge may or may not be present. Infection with C. trachomatis alone does not usually cause much of a discharge. Additionally, 50–70% of the infections due to C. trachomatis in males do not produce any symptoms [29]. Apparently the male urethra contains all the necessary components for antigen presentation and humoral and cellular immune response [34]. On the other hand, urethral infection with C. trachomatis induced weak immunologic responses in humans [30]. In contrast, in a murine model urethral inoculation of C. trachomatis in male mice resulted in a strong humoral and cell-mediated immune response [29]. The immunopathology of urethral infection with C. trachomatis must be further investigated.
Prostatitis
The prostatitis syndrome is one of the most common entities encountered in urologic practice. Classification of the prostatitis syndrome is based on the clinical presentation of the patient, the presence or absence of white blood cells in the expressed prostatic secretion (EPS), and the presence or absence of bacteria in the EPS [37]. Depending upon the duration of symptoms, prostatitis is described as either acute or, where symptoms are present for at least 3 months, as chronic. Referring to the classification of the prostatitis syndrome suggested by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)/National Institutes of Health (NIH), bacterial prostatitis (acute and chronic) is distinguished from chronic pelvic pain syndrome (CPPS) [54]. It is still under debate if and to what extent C. trachomatis can cause prostatitis. In most of the studies, patients with chronic symptoms were included. The definitive association between isolation of C. trachomatis and a prostatic origin is limited by the fact that diagnostic material from the prostate may reflect only urethral contamination [48]. Studies have targeted this problem on the one hand by directly detecting C. trachomatis in specimens obtained via urethra, prostatic biopsies and semen, on the other hand by looking for immune responses (chlamydial antibodies) in prostatic secretions and seminal plasma.
Chlamydia trachomatis in specimens obtained via urethra
Material obtained after passage down the urethra (EPS, urine after prostatic massage, seminal plasma) has been studied [4, 12, 13, 22, 24, 47]. In up to 25% of the cases, chlamydial isolation has been associated with infections to the prostate. In another study using urethral isolation, patients with non-bacterial prostatitis (NIH III) showed C. trachomatis in up to 27% [50]. Therefore, C. trachomatis may originate in the prostate in an unknown percentage of patients with prostatitis symptoms. Because the urethral infection is the origin for ascending infection to the prostate, a discrimination between urethral and prostatic infection is impossible with this approach.
Chlamydia trachomatis in prostatic biopsies
In another approach, the prostatic tissue was obtained from patients with different types of prostatitis. C. trachomatis was detected in 3–30% of the patients [1, 7, 8, 33, 35, 41, 49]. The discrepant results might be due to the different techniques used to retrieve the prostatic tissue. Whereas the tissue from transrectal biopsies, transurethral resection or open surgery might contain epithelial cells from the prostatic urethra (which could have been infected in the course of urethral infection), only in perineal biopsies from the peripheral lobes of the prostate, can urethral contamination be excluded.
Chlamydia trachomatis in semen
It is generally accepted that chlamydia may ascend to the epididymis, may adhere to human spermatozoa and may enter spermatozoa [10, 28, 53]. In any case however, the ejaculate has to pass the urethra, becoming potentially contaminated on its way.
Immune responses to C. trachomatis
Only the MIF test is thought to be able to detect local antibodies on an original type-specified basis. Using the MIF test, 7% of andrological patients had seminal antibodies against C. trachomatis alone [52]. Using the p-ELISA elevated titres of C. trachomatis specific secretory IgA have been identified in acute genital infections [39]. Local secretory IgA-antibodies against C. trachomatis have been evaluated in prostatic secretions and seminal plasma in patients with prostatitis, epididymitis, or infertility [52]. IgA-antibodies in semen is an indicator of genital chlamydial infections. Only some of the IgA-positive specimens however were positive in PCR-investigations [51]. This elucidates the problems of the difficult interpretation of chlamydial antibody findings in this context.
Epididymitis
Chlamydia trachomatis is reported in up to 30% of the patients with epididymitis and occurs more commonly in patients below 35 years of age [55]. The symptoms involve subacute to chronic scrotal pain and epididymis oedema. The symptoms generally persist for a longer time than in patients with epididymitis of another etiology. The occurrence of chlamydial epididymitis is not always preceded by symptoms of urethritis and only in some cases they are accompanied by the increase of polynuclear leukocytes in urethral discharge. Chlamydial epididymitis is of milder course when compared to epididymitis of another etiology [27]. In a male rat model, after inoculation of C. trachomatis in the vas deferens, histological findings included lesions in the epididymides consisting of pyogranulomatous inflammation, abscesses and spermatic granulomas. Infection of the testis by C. trachomatis also occurred and was associated with pyogranulomatous changes. In addition, testicular degeneration, characterized by moderate to severe loss of the germinal epithelium, was noted [16]. Therefore, epididymitis caused by C. trachomatis can cause significant andrological sequelae.
Infertility
Whether infertility in the male could be caused by C. trachomatis has been under debate for years. It has been shown that the in vitro exposure of spermatozoa to EBs of C. trachomatis can lead to sperm death [14]. In vivo analyses have recently shown that C. trachomatis is associated with sperm pathology [46]. In another study, C. trachomatis IgG antibodies in the man of the infertile couple was related to decreased pregnancy rates and to the presence of IgG antibodies in the woman [15]. In this study, there was a high prevalence of asymptomatic persistent infections among the infertile couples. C. trachomatis-antibody testing of both the male and female partner of the couple might therefore be included in the routine infertility work-up in order to enable a more adequate prognosis for the likelihood of a spontaneous pregnancy. Further studies need to investigate, if antibiotic treatment to C. trachomatis IgG-positive infertile patients will increase the couple’s likelihood to achieve pregnancy in spontaneous and/or assisted reproductive cycles [15].
Reactive arthritis and Reiter’s syndrome
The male infection with C. trachomatis can especially lead to reactive arthritis and sometimes even to Reiter’s syndrome. Frequently, the reactive arthritis is seen in young patients before 25 years of age. Predominantly peripheral joints are affected unilaterally in more than 60% [44]. In one study however, C. trachomatis was found in up to 25% of the patients with ankylosing spondylitis [18]. The patients are rheumafactor-negative and HLA-B27 positivity is found in 40–60% of the patients. Whereas in reactive arthritis, due to bacteria other than Chlamydiae, vital organisms will not be found in the affected joints, in patients with reactive arthritis due to C. trachomatis, DNA and mRNA can regularly be isolated [44]. It seems that antibiotic therapy in reactive arthritis due to C. trachomatis will lead to persistence of the otherwise self-limitating disease. It has been shown however that in a population with high prevalence of C. trachomatis infection, the prompt antibiotic treatment of the genital disease can reduce the incidence of reactive arthritis from 37 to 10% [44].
Therapy
European guidelines for the management of chlamydial infection have been issued [42]. The following indications for the treatment have been set up: confirmed oculogenital C. trachomatis infection; infection with C. trachomatis in the partner; if laboratory tests for C. trachomatis are not available in a patient with a confirmed Neisseria gonorrhoeae infection; if laboratory tests for C. trachomatis are not available in a patient with clinical signs of a chlamydial infection. These indications were considered because the treatment of the infected patients prevents important sequelae resulting from the infection and transmission to sexual partners.
Chlamydia are only metabolically active in the host cell and therefore only targeted intracellularly by the antibiotics. Intracellularly accumulated antibiotics are tetracyclines, macrolides and quinolones.
First line regimens include:
-
Azithromycin 1 g orally, single dose, or
-
Doxycycline 100 mg orally twice a day for 7 days
-
Alternative regimens are:
-
Erythromycin base 500 mg orally four times a day for 7 days, or
-
Ofloxacin 200 mg orally twice a day for 7 days, or
-
Roxithromycin 150 mg orally twice a day for 7 days, or
-
Clarithromycin 250 mg orally twice a day for 7 days
Although ofloxacin is generally recommended, levofloxacin exhibits excellent activity against C. trachomatis.
Abstinence from sexual intercourse should last for 7 days and until all current partners have received satisfactory treatment [42].
Prevention
Asymptomatic infections are common and can only be excluded by appropriate laboratory testing. Therefore, these infections can only be detected by screening. There are however no strong data that describe effectiveness of screening for men in reducing transmission to women or in preventing acute infections or complications in men [25]. If symptomatic infection is present, the following points should be considered: laboratory diagnosis to increase the reliability of the clinical diagnosis, which may have serious implications for the patient and their sexual partners. Therapy should be started appropriately as recommended and at the initial consultation, if a diagnosis can be made at that visit, and if epidemiological treatment is indicated as a result of a diagnosis in a sexual partner. Partner notification should be considered in confirmed cases. Follow-up should be done to prove efficacy of the therapy and to decide whether a follow-up testing may be indicated. Epidemiology should be performed to allow greater accuracy in the notification of infections, and in the return of epidemiological data to public health agencies [45].
Conclusion
Chlamydia trachomatis is the most frequent cause for sexually transmitted disease in the European countries. The organism has a intracellular habitat with a very specific life cycle. A variety of diagnostic tests have been developed with different sensitivity and specificity. Interpretation of these tests can sometimes be difficult. Diseases caused by C. trachomatis rank from asymptomatic to severe sequelae. Especially in prostatitis, the exact role is still under debate for the technical difficulties localizing the pathogen to the prostate. For treatment, only some antibiotics are effective because of the intracellular habitat of the pathogen. Prevention of infection is a serious issue and comprises treatment and screening efforts, although screening in the male population has so far not strongly been shown to be effective.
References
Abdelatif OMA, Chandler FW, Mc Guire BS (1991) Chlamydia trachomatis in chronic abacterial prostatitis: demonstration by colorimetric in situ hybridization. Hum Pathol 22:41–44
Black CM (1997) Current methods of laboratory diagnosis of Chlamydia trachomatis infections. Clin Microbiol Rev 10:160–183
Brunelle BW, Nicholson TL, Stephens RS (2004) Microarray-based genomic surveying of gene polymorphisms in Chlamydia trachomatis. Genome Biol 5:R42
Bruce AW, Reid G (1989) Prostatitis associated with Chlamydia trachomatis in 6 patients. J Urol 142:1006–1007
Centers for disease control and prevention (1991) Sexually transmitted diseases clinical practice guidelines. centers for disease control and prevention, Atlanta, Georgia
Centers for disease control and prevention (2002) Division of STD prevention. Screening tests to detect Chlamydia trachomatis and Neisseria gonorrhoeae infections. Centers for disease control and prevention, Atlanta, Georgia. http://www.cdc.gov/STD/LabGuidelines/3-LG.htm
Corradi Gy, Bucsek M, Panovics J et al (1996) Detection of Chlamydia trachomatis in the prostate by in-situ hybridization and by transmission electron microscopy. Int J Androl 19:109–112
Doble A, Thomas BJ, Walker MM, Harris JR, Witherow RO’N, Tayler-Robinson D (1989) The role of Chlamydia trachomatis in chronic abacterial prostatitis: a study using ultrasound guided biopsy. J Urol 141:332–333
Domeika M, Bassiri M, Butrimiene I, Venalis A, Rancev J, Vasjanova V (1999) Evaluation of vaginal introital sampling as an alternative approach for the detection of genital chlamydia trachomatis infection in women. Acta Obstet Gynecol Scand 78:131–136
Erbengi T (1993) Ultrastructural observations on the entry of C. trachomatis into human spermatozoa. Hum Reprod 8:416–421
Fioravante FC, Costa Alves MF, Guimaraes EM, Turchi MD, Freitas HA, Domingos LT (2005) Prevalence of Chlamydia trachomatis in asymptomatic Brazilian military conscripts. Sex Transm Dis 32:165–169
Gümüs B, Sengil AZ, Solak M, Fistik T, Alibeyx E, Cakmak EA et al (1997) Evaluation of non-invasive clinical samples in chronic chlamydial prostatitis by using in situ hybridization. Scand J Urol Nephrol 31:449–451
Hequing G, Gongeheng L, Qijun Z, Xulin X (1997) Detection of Chlamydia trachomatis by polymerase chain reaction assay in nonbacterial prostatitis. Chin Med J 110:177–179
Hosseinzadeh S, Pacey AA, Eley A (2003) Chlamydia trachomatis-induced death of human spermatozoa is caused primarily by lipopolysaccharide. J Med Microbiol 52:193–200
Idahl A, Boman J, Kumlin U, Olofsson JI (2004) Demonstration of Chlamydia trachomatis IgG antibodies in the male partner of the infertile couple is correlated with a reduced likelihood of achieving pregnancy. Hum Reprod 19:1121–1126
Jantos C, Baumgartner W, Durchfeld B, Schiefer HG (1992) Experimental epididymitis due to Chlamydia trachomatis in rats. Infect Immun 60:2324–2328
Jones RB, Katz BP, VanderPol B, Caine VA, Batteiger BE, Newhall WJ (1986) Effect of blind passage and multiple sampling on recovery of Chlamydia trachomatis from urogenital specimens. J Clin Microbiol 24:1029–1033
Lange U, Berliner M, Weidner W, Schiefer HG, Schmidt KL, Federlin K (1996) Ankylosing spondylitis and urogenital infection: diagnosis of urologic infection and correlation with rheumatologic findings. Z Rheumatol 55:249–255
Low N, Egger M, Simms I, Herrmann B (1999) Contrasting trends in ratea of genital chlamydial infection and ectoopic pregnancy in South East Thames Region, England and Uppsala County, Sweden: ecological study. J Epidemiol Community Health 53:438–439
Mahony J, Chong S, Jang D et al (1998) Urine specimens from pregnant and nonpregnant women inhibitory to amplification of chlamydia trachomatis nucleic acid by PCR, ligase chain reaction, and transcription—mediated amplification: identification of urinary substances associated with inhibition and removal of inhibitory activity. J Clin Microbiol 36:3122–3126
Mamat U, Baumann M, Schmidt G, Brade H (1993) The genus-specific lipopolysaccharide epitope of chlamydia is assembled in C. psittaci and C. trachomatis by glycosyltransferase of low homology. Mol Microbiol 10:935–941
Mazzoli S, Bani D, Salvi A, Ramaciotti I, Romeo C, Bani T (2000) In vivo evidence of Chlamydia trachomatis muniature reticulary bodies (MRB) as persistence markers in chronic prostatitis. In: Proceedings of the fourth meeting of the European society for Chlamydia research (Abstract) Helsinki
Meijer A, Morré SA, Van Den Brule AJC, Savelkoul PHM, Ossewaarde JM (1999) Genomic relatedness of Chlamydia isolates determined by amplified fragment length polymorphism analysis. J Bacteriol 181:4469–4475
Mutlu N, Mutlu B, Culha M, Hamsioglu Z, Demirtas M, Gökalp A (1998) The role of Chlamydia trachomatis in patients with non-bacterial prostatitis. Int J Clin Pract 52:540–541
Nelson HD, Somath S, Helfand M (2001) Screening for chlamydial infection. Systematic Evidence Review No. 3 (Prepared by the Oregon Health Sciences University Evidence-based Practice Center under Contract No 290-97-0018). AHRQ Publication No. 01-S003, Agency for Healthcare Research and Quality, Rockville, MD
Nicholson TL, Olinger L, Chong K, Schoolnik G, Stephens RS (2003) Global stage-specific gene regulation during the developmental cycle of Chlamydia trachomatis. J Bacteriol 185:3179–3189
Ostaszewska I, Zdrodowska-Stefanow B, Darewicz B, Darewicz J, Badyda J, Pucilo K, Bulhak V, Szczurzewski M (2000) Role of Chlamydia trachomatis in epididymitis. Part II: Clinical diagnosis. Med Sci Monit 6:1119–1121
Paavonen J, Eggert-Kruse WC (1999) C. trachomatis impact on human reproduction. Hum Reprod Update 5:433–447
Pal S, Peterson EM, de la Maza LM (2004) New murine model for the study of Clamydia trachomatis genitourinary tract infections in males. Infect Immun 72:4210–4216
Pate MS, Hedges SR, Sibley DA, Russell MW, Hook EW, Mestescky J (2001) Urethral cytokine and immune response in Chlamydia trachomatis-infected males. Infect Immun 69:5203–5206
Petersen EE, Obermann K, Graf von der Schulenburg JM (1998) Health care and preventive measures via chlamydia screening. Geburtsh Frauenheilk 58:408–414
Petzold D, Gross G (eds) (2001) Diagnostik und Therapie sexuell übertragbarer Krankheiten. Leitlinien 2001 der Deutschen STD-Gesellschaft. Springer, Berlin Heidelberg New York
Poletti F, Medici MC, Alinovi A, et al (1985) Isolation of Chlamydia trachomatis from the prostatic cells in patients affected by nonacute abacterial prostatitis. J Urol 134:691–693
Pudney J, Anderson DJ (1995) Immunobiology of the human penile urethra. Am J Pathol 147:155–165
Pust R, Schäfer R, Stumpf CH, Leitenberger A, Engstfeld JE, Meier-Ewert H (1986) Urethritis posterior. In: Weidner W, Brunner H, Krause W, Rothauge CF (eds) Therapy of prostatitis. Zuckschwerdt, München, pp 102–109
Rockey DD, Lenart J, Stephens RS (2000) Genome sequencing and our understanding of chlamydiae. Infect Immun 68:5473–5479
Schaeffer AJ (1999) Prostatitis: US perspective. Int J Antimicrob Agents 11:205–211
Schillinger JA, Dunne EF, Chapin JB, Ellen JM, Gaydos CA, Willard NJ, Kent CK, Marrazzo JM, Klausner JD, Rietmeijer CA, Markowitz LE (2005) Prevalence of Chlamydia trachomatis infection among men screened in 4 U.S. cities. Sex Transm Dis 32:74–77
Schuppe HC, Bispink G, Peet DJ, Propping D, Böttcher M, De Hlaff S (2000) The significance of antibodies against C. trachomatis I seminal plasma (Abstract). In: Proceedings of the fourth meeting of the European society for Chlamydia research (Abstract). Helsinki
Shafer MA, Pantell RH, Schachter J (1999) Is the routine pelvic examination needed with the advent of urine-based screening for sexually transmitted diseases? Arch Pediatr Adolesc Med 152:119–125
Shurbaji MS, Gupta PK, Myers J (1988) Immunohistochemical demonstration of chlamydial antigens in association with prostatitis. Mod Pathol 1:348–351
Stary A (2001) European guideline for the management of chlamydial infefction. Int J STD AIDS 12(Suppl 3):30–33
Stephens RS (2003) The cellular paradigm of chlamydial pathogenesis. Trends Microbiol 11:44–51
Straube E (2004) Chlamydien. In: Adam D, Doerr HW, Link H, Lode H (eds) Die infektiologie. Springer, Berlin Germany
Van Voorst Vader, Radcliffe KW (2001) European guideline for the organization of a consultation for sexually transmitted diseases. Int J STD AIDS 12(Suppl 3):4–6
Veznik Z, Pospisil L, Svecova D, Zajicova A, Unzeitig V (2004) Chlamydiae in the ejaculate: their influence on the quality and morphology of sperm. Acta Obstet Gynecol Scand 83:656–660
Weidner W, Arens M, Kraus H, Schiefer HG, Ebner H (1984) Chlamydia trachomatis in abacterial prostatitis: microbiological, cytological and serological studies. Urol Int 38:146–149
Weidner W, Schiefer HG (1985) Isolation of C. trachomatis from the prostatic cells in patients affected by non-acute abacterial prostatitis. J Urol 134:690
Weidner W, Schiefer HG, Krauss H, Jantos C, Friedrich HJ, Altmannsberger M (1991) Chronic prostatitis a thorough search for etiologically involved microorganisms in 1461 patients. Infection 19(Suppl 3):119–125
Weidner W, Schiefer HG (1995) Inflammatory disease of the prostate: frequency and pathogenesis. In: Garraway M (ed) Epidemiology of prostate disease. Springer, Berlin Heidelberg New York, pp 85–93
Weidner W, Floren E, Zimmermann O, Thiele D, Ludwig M (1996) Chlamydial antibodies in semen: search for ‘silent’ chlamydial infections in asymptomatic andrological patients. Infection 24:309–313
Weidner W, Diemer Th, Huwe P, Rainer H, Ludwig M (2002) The role of Chlamydia trachomatis in prostatitis. Int J Antimicrob Agents 19:466–470
Wølner-Hanssen P, Márdh PA (1984) In vitro tests of the adherence of C. trachomatis to human spermatozoa. Fertil Steril 42:102–107
Workshop Committee of the National Institute of Diabetes and Digestive and Kidney Disease (NIDDK) (1995) Chronic Prostatitis Workshop, Bethesda, MD, 7–8 December, 1995
Zdrodowska-Stefanow B, Ostaszewska I, Darewicz B, Darewicz J, Badyda J, Pucilo K, Bulhak V, Szczurzewski M (2000) Role of Chlamydia trachomatis in epididymitis. Part I: Direct and serologic diagnosis. Med Sci Monit 6:1113–1118
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wagenlehner, F.M.E., Weidner, W. & Naber, K.G. Chlamydial infections in urology. World J Urol 24, 4–12 (2006). https://doi.org/10.1007/s00345-005-0047-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-005-0047-x