Abstract
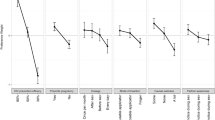
Conjoint Analysis (CJA), a statistical market-based technique that assesses the value consumers place on product characteristics, may be used to predict acceptability of hypothetical products. Rectal Microbicides (RM)—substances that would prevent HIV infection during receptive anal intercourse—will require acceptability data from potential users in multiple settings to inform the development process by providing valuable information on desirable product characteristics and issues surrounding potential barriers to product use. This study applied CJA to explore the acceptability of eight different hypothetical RM among 128 MSM in Lima and Iquitos, Peru; Guayaquil, Ecuador; and Rio de Janeiro, Brazil. Overall RM acceptability was highest in Guayaquil and lowest in Rio. Product effectiveness had the greatest impact on acceptability in all four cities, but the impact of other product characteristics varied by city. This study demonstrates that MSM from the same region but from different cities place different values on RM characteristics that could impact uptake of an actual RM. Understanding specific consumer preferences is crucial during RM product development, clinical trials and eventual product dissemination.
Resumen
El Análisis Conjunto (CJA por sus siglas en inglés) es una técnica estadística de mercadotecnia que sirve para evaluar la valoración que los consumidores otorgan a las características de un producto, y que puede ser usada para predecir la aceptabilidad de productos hipotéticos. Para el desarrollo de microbicidas rectales (MR)—sustancias que podrían prevenir la infección por VIH durante el coito anal receptivo—es necesario contar con datos de aceptabilidad, características deseadas y probables barreras para el empleo de MR por usuarios potenciales, en múltiples escenarios. Este estudio aplica CJA para explorar la aceptabilidad de ocho diferentes MR hipotéticos entre 128 HSH en Lima e Iquitos, Perú; Guayaquil, Ecuador; y Río de Janeiro, Brasil. En general, la más alta aceptabilidad se dio en Guayaquil y la más baja en Río. La eficacia del producto tuvo el mayor impacto sobre la aceptabilidad en las cuatro ciudades, pero el impacto de otras características del producto varió por ciudades. Este estudio demuestra que los HSH, aunque son de la misma región, pero de diferentes ciudades, otorgan valores distintos a las características de los MR, lo cual podría afectar el uso de un MR real. Es crucial entender las preferencias específicas de los consumidores durante la investigación, desarrollo y eventual difusión de los MR.
Similar content being viewed by others
References
Abdool Karim Q, Abdool Karim SS, Frohlich JA, et al. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science. 2010;329(5996):1168–74.
Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99.
University of Washington International Clinical Research Center: partners PrEP study. Pivotal study finds that HIV medications are highly effective as prophylaxis against HIV infection in men and women in Africa. 2011; Available at: http://depts.washington.edu/uwicrc/research/studies/files/PrEP_PressRelease-UW_13Jul2011.pdf. Accessed 15 July 2011.
Centers for Disease Control and Prevention. CDC trial and another major study find PrEP can reduce risk of HIV infection among Heterosexuals. 2011. Available at: http://www.cdc.gov/nchhstp/newsroom/PrEPHeterosexuals.html. Accessed 15 July 2011.
Joglekar NS, Joshi SN, Deshpande SS, Parkhe AN, Katti UR, Mehendale SM. Acceptability and adherence: findings from a Phase II study of a candidate vaginal microbicide, ‘Praneem polyherbal tablet’, in Pune, India. Trans R Soc Trop Med Hyg. 2010;104(6):412–5.
McGowan I. Rectal microbicides: can we make them and will people use them? AIDS Behav. 2011;15(Suppl 1):S66–71.
International Rectal Microbicides Advocates (IRMA). From promise to product: advancing rectal microbicide research and advocacy, Chicago; 2010.
Carballo-Diéguez A, Dolezal C, Bauermeister JA, O’Brien W, Ventuneac A, Mayer K. Preference for gel over suppository as delivery vehicle for a rectal microbicide: results of a randomised, crossover acceptability trial among men who have sex with men. Sex Transm Infect. 2008;84(6):483–7.
Carballo-Diéguez A, Bauermeister JA, Ventuneac A, Dolezal C, Balan I, Remien RH. The use of rectal douches among HIV-uninfected and infected men who have unprotected receptive anal intercourse: implications for rectal microbicides. AIDS Behav. 2008;12(6):860–6.
Carballo-Diéguez A, Bauermeister J, Ventuneac A, Dolezal C, Mayer K. Why rectal douches may be acceptable rectal-microbicide delivery vehicles for men who have sex with men. Sex Transm Dis. 2009;37(4):228–9.
Carroll J, Green P. Psychometric methods in marketing research: part I, conjoint analysis. J Mark Res. 1995;XXXII:385–9.
Green P, Rao V. Conjoint measurement for quantifying judgmental data. J Mark Res. 1971;8(3):355–63.
Green P, Srinivasan V. Conjoint analysis in marketing research: new developments and directions. J Mark Res. 1990;54:3–19.
Marshall P, Bradlow E. A unified approach to conjoint analysis models. J Am Stat Assoc. 2002;97(459):674–82.
Beusterien KM, Dziekan K, Flood E, Harding G, Jordan JC. Understanding patient preferences for HIV medications using adaptive conjoint analysis: feasibility assessment. Value Health. 2005;8(4):453–61.
Akkazieva B, Gulacsi L, Brandtmuller A, Pentek M, Bridges JF. Patients’ preferences for healthcare system reforms in Hungary: a conjoint analysis. Appl Health Econ Health Policy. 2006;5(3):189–98.
Aristides M, Chen J, Schulz M, Williamson E, Clarke S, Grant K. Conjoint analysis of a new chemotherapy: willingness to pay and preference for the features of raltitrexed versus standard therapy in advanced colorectal cancer. Pharmacoeconomics. 2002;20(11):775–84.
Bhargava JS, Bhan-Bhargava A, Foss AJ, King AJ. Views of glaucoma patients on provision of follow-up care; an assessment of patient preferences by conjoint analysis. Br J Ophthalmol. 2008;92(12):1601–5.
Bishai D, Brice R, Girod I, Saleh A, Ehreth J. Conjoint analysis of French and German parents’ willingness to pay for meningococcal vaccine. Pharmacoeconomics. 2007;25(2):143–54.
Bishop AJ, Marteau TM, Armstrong D, et al. Women and health care professionals’ preferences for Down’s syndrome screening tests: a conjoint analysis study. BJOG. 2004;111(8):775–9.
Costa ML, de Cassia Braga Ribeiro K, Machado MA, Costa AC, Montagnini AL. Prognostic score in gastric cancer: the importance of a conjoint analysis of clinical, pathologic, and therapeutic factors. Ann Surg Oncol. 2006;13(6):843–50.
Cunningham CE, Deal K, Rimas H, Chen Y, Buchanan DH, Sdao-Jarvie K. Providing information to parents of children with mental health problems: a discrete choice conjoint analysis of professional preferences. J Abnorm Child Psychol. 2009;37(8):1089–102.
Fisher K, Orkin F, Frazer C. Utilizing conjoint analysis to explicate health care decision making by emergency department nurses: a feasibility study. Appl Nurs Res. 2010;23(1):30–5.
Ryan M, Farrar S. Using conjoint analysis to elicit preferences for health care. BMJ. 2000;320(7248):1530–3.
Lancsar EJ, Hall JP, King M, et al. Using discrete choice experiments to investigate subject preferences for preventive asthma medication. Respirology. 2007;12(1):127–36.
Stone VE, Jordan J, Tolson J, Miller R, Pilon T. Perspectives on adherence and simplicity for HIV-infected patients on antiretroviral therapy: self-report of the relative importance of multiple attributes of highly active antiretroviral therapy (HAART) regimens in predicting adherence. J Acquir Immune Defic Syndr. 2004;36(3):808–16.
Newman PA, Duan N, Lee SJ, et al. HIV vaccine acceptability among communities at risk: the impact of vaccine characteristics. Vaccine. 2006;24(12):2094–101.
Galea J, Kinsler J, Salazar X, et al. Acceptability of pre-exposure prophylaxis (PrEP) as an HIV prevention strategy: barriers and facilitators to PrEP uptake among at-risk Peruvian populations. Int J STD AIDS. 2010;22:256–62.
Lancsar E, Savage E. Deriving welfare measures from discrete choice experiments: inconsistency between current methods and random utility and welfare theory. Health Econ. 2004;13(9):901–7.
Hunink M, Glasziou P, Siegel J, et al. Decision making in health and medicine: integrating evidence and values. Cambridge: Cambridge University Press; 2001.
UNAIDS. Global report: UNAIDS report on the global AIDS epidemic 2010. Geneva: UNAIDS. Accessed 10 April 2011.
Baral S, Sifakis F, Cleghorn F, Beyrer C. Elevated risk for HIV infection among men who have sex with men in low- and middle-income countries 2000–2006: a systematic review. PLoS Med. 2007;4(12):e339.
Gray RH, Wawer MJ, Brookmeyer R, et al. Probability of HIV-1 transmission per coital act in monogamous, heterosexual, HIV-1-discordant couples in Rakai, Uganda. Lancet. 2001;357(9263):1149–53.
Vittinghoff E, Douglas J, Judson F, McKirnan D, MacQueen K, Buchbinder SP. Per-contact risk of human immunodeficiency virus transmission between male sexual partners. Am J Epidemiol. 1999;150(3):306–11.
Foss A, Johnson H, Prudden H, et al. Modelling the potential impact on HIV transmission of a rectal microbicide used by men who have sex with men and the effects of condom substitution. Microbicides. Pittsburgh, 2010 [abstract WEPE0340].
Sánchez J. Cutting the edge of the HIV epidemic among MSM. Presented at: The Center for HIV Identification, Prevention, and Treatment Services (CHIPTS). The future direction of male circumcision in HIV prevention working conference; April 9, 2007; Los Angeles. http://chipts.ucla.edu/TEMPMAT/MaleCirc2007/Sanchez%20LA.pdf. Accessed 15 July 2011.
Holmes WR, Maher L, Rosenthal SL. Attitudes of men in an Australian male tolerance study towards microbicide use. Sex Health. 2008;5(3):273–8.
Orme B. Getting started with conjoint analysis: strategies for product design and pricing research. 2nd ed. Madison: Research Publishers LLC; 2010.
Carballo-Diéguez A, Exner T, Dolezal C, Pickard R, Lin P, Mayer KH. Rectal microbicide acceptability: results of a volume escalation trial. Sex Transm Dis. 2007;34(4):224–9.
Pickett J, LeBlanc MA, Gorbach P, Murphy R, Javanbakht M. International lubricant use behaviors for anal intercourse. XVII international AIDS conference. Mexico City, 2008. [abstract WEPE0275].
Anton P, Saunders T, Adler A, et al. A phase 1 safety and acceptability study of the UC-781 microbicide gel applied rectally in HIV seronegative adults: an interim safety report at 50% completion. Microbicides. New Delhi, 2008. [abstract BO5-290].
Kinsler JJ, Galea JT, Peinado J, Segura P, Montano SM, Sánchez J. Lubricant use among men who have sex with men reporting receptive anal intercourse in Peru: implications for rectal microbicides as an HIV prevention strategy. Int J STD AIDS. 2010;21(8):567–72.
Anton P, Cranston R, Carballo-Diéguez A, et al. RMP-02/MTN-006: a phase 1 placebo-controlled trial of rectally applied 1% vaginal TFV gel with comparison to oral TDF. The 18th conference on retroviruses and opportunistic infections, Boston, USA; 2011.
Galea J, Kinsler J, Segura P, Peinado J, Sánchez J. The use of rectal douches among peruvian MSM: implications for rectal microbicides. Microbicides, Pittsburgh, 2010. [abstract 162].
Saethre EJ, Stadler J. Gelling medical knowledge: innovative pharmaceuticals, experience, and perceptions of efficacy. Anthropol Med. 2010;17(1):99–111.
Vail JG, Cohen JA, Kelly KL. Improving topical microbicide applicators for use in resource-poor settings. Am J Public Health. 2004;94(7):1089–92.
Cohen JA, Steele MS, Urena FI, Beksinska ME. Microbicide applicators: understanding design preferences among women in the dominican republic and South Africa. Sex Transm Dis. 2007;34(1):15–9.
Cassell MM, Halperin DT, Shelton JD, Stanton D. Risk compensation: the Achilles’ heel of innovations in HIV prevention? BMJ. 2006;332(7541):605–7.
Pinkerton SD. Sexual risk compensation and HIV/STD transmission: empirical evidence and theoretical considerations. Risk Anal. 2001;21(4):727–36.
Newman PA, Duan N, Rudy ET, Roberts KJ, Swendeman D. Posttrial HIV vaccine adoption: concerns, motivators, and intentions among persons at risk for HIV. J Acquir Immune Defic Syndr. 2004;37(3):1393–403.
Acknowledgments
This research was funded by the UCLA AIDS Institute/UCLA Program in Global Health seed grant in international prevention and policy research for HIV/AIDS (# AI28697). In addition to the study volunteers who gave their time to this study, the authors would like to thank Dr. Peter Anton, Dr. Alex Carballo-Diéguez, Dr. Kenneth Mayer and Dr. Ian McGowan for lending their expertise in the CJA attribute selection and Site Coordinators Patricia Segura and Robert De La Grecca (Lima), Lucia Ruiz (Iquitos), Luis Fernando Galarza (Guayaquil), and Nilo Martinez Fernandes (Rio) who managed study implementation in each country.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kinsler, J.J., Cunningham, W.E., Nureña, C.R. et al. Using Conjoint Analysis to Measure the Acceptability of Rectal Microbicides Among Men Who Have Sex with Men in Four South American Cities. AIDS Behav 16, 1436–1447 (2012). https://doi.org/10.1007/s10461-011-0045-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-011-0045-5