Abstract
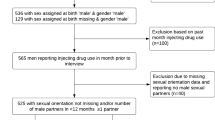
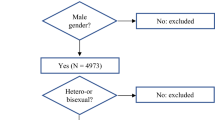
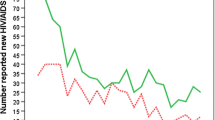
Injecting drug use is commonly reported among gay and bisexual men in Australia. We examined the prevalence and covariates of injecting drug use among men participating in the Sydney Gay Community Periodic Survey between 2004–06 and 2011. In 2004–06, data was collected about which drugs were injected, while in 2011, data was collected about hepatitis C (HCV) and esoteric sexual practices. In 2004–06, 5.6 % of men reported injecting drugs in the previous 6 months; 3.4 % reported methamphetamine injection and 0.4 % heroin injection. In 2011, men who injected drugs were less likely to be employed full-time, and more likely to be HCV-positive, HIV-positive, to have used party drugs for sex, and to have engaged in esoteric sexual practices. The strong associations between injecting drug use, sexual risk practices and blood-borne virus infection suggests the need for combined sexual health and harm reduction services for gay and bisexual men who inject drugs.
Resumen
Por lo general, en Australia, se suele registrar un alto índice de prevalencia de consumo de drogas por vía intravenosa entre hombres homosexuales y bisexuales. En el presente estudio, se analizaron la prevalencia y las covariables del consumo de drogas intravenosas entre los hombres homosexuales y bisexuales que participaron en la Encuesta periódica de la comunidad homosexual de Sídney (Sydney Gay Community Periodic Survey) entre 2004–06 y 2011. Los datos del período 2004–06 incluyen información específica sobre qué drogas fueron consumidas por vía intravenosa, mientras que en 2011 se recolectaron datos específicos sobre hepatitis C (VHC) y prácticas sexuales esotéricas. En 2004–06, el 5,6 % de los hombres consultados dijo haber consumido drogas intravenosas durante los últimos seis meses, de los cuales el 3,4 y el 0,4 % refirió el consumo de metanfetaminas y heroína por vía intravenosa, respectivamente. En 2011, el 5,0 % de los participantes dijo haber consumido drogas intravenosas durante los últimos seis meses. En 2011, dichos consumidores tenían menos probabilidades de poseer un trabajo de tiempo completo y más probabilidades de presentar VHC positivo y VIH positivo, de haber consumido drogas recreacionales para tener relaciones sexuales y de haber participado en prácticas sexuales esotéricas. La estrecha relación existente entre el consumo de drogas intravenosas, las prácticas sexuales de riesgo y las infecciones víricas de transmisión hemática sugiere la necesidad de implementar servicios combinados de salud sexual y de reducción del daño para hombres homosexuales y bisexuales consumidores de drogas intravenosas.
Similar content being viewed by others
References
Knox S, Kippax S, Crawford J, Prestage G, Van De Ven P. Non-prescription drug use by gay men in Sydney, Melbourne and Brisbane. Drug Alcohol Rev. 1999;18:425–33.
Van de Ven P, Kippax S, Crawford J, Rodden P. Injecting drug use and knowledge and self-report of hepatitis C among Australian gay and homosexually active men. Drug Alcohol Rev. 1999;18:271–7.
Greenwood GL, White EW, Page-Shafer K, Bein E, Osmond DH, Paul J, et al. Correlates of heavy substance use among young gay and bisexual men: the San Francisco Young Men’s Health Study. Drug Alcohol Depend. 2001;61:105–12.
Prestage G, Fogarty A, Rawstorne P, Grierson J, Zablotska I, Grulich A, et al. Use of illicit drugs among gay men living with HIV in Sydney. AIDS. 2007;21:S49–55.
Sullivan PS, Nakashima AK, Purcell DW, Ward JW. Geographic differences in noninjection and injection substance use among HIV-seropositive men who have sex with men: Western United States versus other regions. JAIDS. 1998;19:266–73.
Ibanez GE, Purcell DW, Stall R, Parsons JT, Gomez CA. Sexual risk, substance use, and psychological distress in HIV-positive gay and bisexual men who also inject drugs. AIDS. 2005;19:S49–55.
Lea T, Prestage G, Mao L, Zablotska I, De Wit J, Holt M. Trends in drug use among gay and bisexual men in Sydney, Melbourne and Queensland, Australia. Drug Alcohol Rev. doi: 10.1111/j.1465-3362.2012.00494.x (in press).
Australian Institute of Health and Welfare. 2010 National Drug Strategy Household Survey report. Drug statistics series no. 25. Cat. no. PHE 145. Canberra: AIHW, 2011.
Aceijas C, Rhodes T. Global estimates of prevalence of HCV infection among injecting drug users. Int J Drug Policy. 2007;18:352–8.
Mathers BM, Degenhardt L, Phillips B, Wiessing L, Hickman M, Strathdee SA, et al. Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. Lancet. 2008;372:1733–45.
Theodorou S, Haber PS. The medical complications of heroin use. Curr Opin Psychiatr. 2005;18:257–63.
Strang J, Bearn J, Farrell M, Finch E, Gossop M, Griffiths P, et al. Route of drug use and its implications for drug effect, risk of dependence and health consequences. Drug Alcohol Rev. 1998;17:197–211.
Danta M, Rodger AJ. Transmission of HCV in HIV-positive populations. Curr Opin HIV AIDS. 2011;6:451.
van de Laar TJW, Matthews GV, Prins M, Danta M. Acute hepatitis C in HIV-infected men who have sex with men: an emerging sexually transmitted infection. AIDS. 2010;24:1799–812.
Iversen J, Maher L. Australian Needle and Syringe Program National Data Report 2007–2011. Sydney: The Kirby Institute, The University of New South Wales; 2012.
The Kirby Institute. HIV, viral hepatitis and sexually transmissible infections in Australia: Annual Surveillance Report 2011. Sydney: The Kirby Institute, The University of New South Wales; 2011.
Grulich AE, Visser RO, Smith A, Rissel CE, Richters J. Sex in Australia: injecting and sexual risk behaviour in a representative sample of adults. Aust NZ J Public Health. 2003;27:242–50.
Bull SS, Piper P, Rietmeijer C. Men who have sex with men and also inject drugs: profiles of risk related to the synergy of sex and drug injection behaviors. J Homosex. 2002;42:31–51.
Kral AH, Lorvick J, Ciccarone D, Wenger L, Gee L, Martinez A, et al. HIV prevalence and risk behaviors among men who have sex with men and inject drugs in San Francisco. J Urban Health. 2005;82:i43–50.
Murnane A, Smith A, Crompton L, Snow P, Munro G. Beyond perceptions: a report on alcohol and other drug use among gay, lesbian, bisexual and queer communities in Victoria. Melbourne: Australian Drug Foundation; 2000.
Inglez-Dias A, Hahn JA, Lum PJ, Evans J, Davidson P, Page-Shafer K. Trends in methamphetamine use in young injection drug users in San Francisco from 1998 to 2004: the UFO Study. Drug Alcohol Rev. 2008;27:286–91.
Roxburgh A, Degenhardt L, Breen C. Changes in patterns of drug use among injecting drug users following changes in the availability of heroin in New South Wales Australia. Drug Alcohol Rev. 2004;23:287–94.
NTA. Injecting drug use in England: a declining trend. London: National Treatment Agency for Substance Misuse, National Health Service, UK; 2010.
Stafford J, Burns L. Australian Drug Trends 2011. Findings from the Illicit Drug Reporting System (IDRS). Australian drug trend series no. 73. Sydney: National Drug and Alcohol Research Centre, The University of New South Wales; 2012.
Dowsett GW, Wain D, Keys D. Good gay men don’t get “messy”: injecting drug use and gay community. Sex Res Social Policy. 2005;2:22–36.
Hurley M, Prestage G. Intensive sex partying amongst gay men in Sydney. Cult Health Sex. 2009;11:597–610.
Slavin S. Crystal methamphetamine use among gay men in Sydney. Contemp Drug Probl. 2004;31:425–65.
Slavin S. Drugs, space, and sociality in a gay nightclub in Sydney. J Contemp Ethnogr. 2004;33:265–95.
Halkitis PN, Mukherjee PP, Palamar JJ. Multi-level modeling to explain methamphetamine use among gay and bisexual men. Addiction. 2007;102:S76–83.
Semple SJ, Patterson TL, Grant I. Motivations associated with methamphetamine use among HIV+ men who have sex with men. J Subst Abuse Treat. 2002;22:149–56.
Reback CJ. The social construction of a gay drug: methamphetamine use among gay and bisexual males in Los Angeles. Los Angeles: AIDS Coordinator; 1997.
Green AI, Halkitis PN. Crystal methamphetamine and sexual sociality in an urban gay subculture: an elective affinity. Cult Health Sex. 2006;8:317–33.
Ghanem A, Little SJ, Drumright L, Liu L, Morris S, Garfein RS. High-risk behaviors associated with injection drug use among recently HIV-infected men who have sex with men in San Diego, CA. AIDS Behav. 2011;15:1561–9.
Rawstorne P, Digiusto E, Worth H, Zablotska I. Associations between crystal methamphetamine use and potentially unsafe sexual activity among gay men in Australia. Arch Sex Behav. 2007;36:646–54.
Bolding G, Hart G, Sherr L, Elford J. Use of crystal methamphetamine among gay men in London. Addiction. 2006;101:1622–30.
Colfax GN, Vittinghoff E, Husnik MJ, McKirnan D, Buchbinder S, Koblin B, et al. Substance use and sexual risk: a participant- and episode-level analysis among a cohort of men who have sex with men. Am J Epidemiol. 2004;159:1002–12.
Koblin B, Murrill C, Camacho M, Xu G, Liu K, Raj-Singh S, et al. Amphetamine use and sexual risk among men who have sex with men: results from the National HIV Behavioral Surveillance study-New York City. Subst Use Misuse. 2007;42:1613–28.
Plankey MW, Ostrow DG, Stall R, Cox C, Li X, Peck JA, et al. The relationship between methamphetamine and popper use and risk of HIV seroconversion in the multicenter AIDS cohort study. J AIDS. 2007;45:85–92.
Semple SJ, Patterson TL, Grant I. A comparison of injection and non-injection methamphetamine-using HIV positive men who have sex with men. Drug Alcohol Depend. 2004;76:203–12.
Ellard J. ‘There is no profile it is just everyone’: the challenge of targeting hepatitis C education and prevention messages to the diversity of current and future injecting drug users. Int J Drug Policy. 2007;18:225–34.
Southgate E, Hopwood M. Mardi Gras says ‘Be drug free’: accounting for resistance, pleasure and the demand for illicit drugs. Health. 1999;3:303–16.
Southgate E, Hopwood M. The role of folk pharmacology and lay experts in harm reduction: Sydney gay drug using networks. Int J Drug Policy. 2001;12:321–35.
Zablotska IB, Kippax S, Grulich A, Holt M, Prestage G. Behavioural surveillance among gay men in Australia: methods, findings and policy implications for the prevention of HIV and other sexually transmissible infections. Sex Health. 2011;8:272–9.
Kippax S, Campbell D, Van de Ven P, Crawford J, Prestage G, Knox S, et al. Cultures of sexual adventurism as markers of HIV seroconversion: a case control study in a cohort of Sydney gay men. AIDS Care. 1998;10:677–88.
Zablotska I, Prestage G, Hull P, Crawford J, Kippax S, Sutherland R, et al. Sydney Gay Community Periodic Survey: February 1996 to February 2006. Sydney: National Centre in HIV Social Research and National Centre in HIV Epidemiology and Clinical Research, The University of New South Wales; 2006.
Kaye S, Darke S. A comparison of the harms associated with the injection of heroin and amphetamines. Drug Alcohol Depend. 2000;58:189–95.
Mansergh G, Colfax GN, Marks G, Rader M, Guzman R, Buchbinder S. The circuit party men’s health survey: findings and implications for gay and bisexual men. Am J Public Health. 2001;91:953–8.
Prestage G, Down I, Grulich A, Zablotska I. Sex partying among gay men in Sydney, Melbourne and Brisbane, Australia. AIDS Behav. 2011;15:298–304.
Prestage G, Grierson J, Bradley J, Hurley M, Hudson J. The role of drugs during group sex among gay men in Australia. Sex Health. 2009;6:310–7.
Mattison AM, Ross MW, Wolfson T, Franklin D. Circuit party attendance, club drug use, and unsafe sex in gay men. J Subst Abuse. 2001;13:119–26.
Urbanus AT, van de Laar TJ, Stolte IG, Schinkel J, Heijman T, Coutinho RA, et al. Hepatitis C virus infections among HIV-infected men who have sex with men: an expanding epidemic. AIDS. 2009;23:F1–7.
Bottieau E, Apers L, Van Esbroeck M, Vandenbruaene M, Florence E. Hepatitis C virus infection in HIV-infected men who have sex with men: sustained rising incidence in Antwerp, Belgium, 2001–2009. Eurosurveillance. 2010;15:19673.
Jin F, Prestage GP, Matthews G, Zablotska I, Rawstorne P, Kippax SC, et al. Prevalence, incidence and risk factors for hepatitis C in homosexual men: data from two cohorts of HIV-negative and HIV-positive men in Sydney, Australia. Sex Transm Infect. 2010;86:25–8.
Kim JH, Psevdos G, Suh J, Sharp VL. Co-infection of hepatitis B and hepatitis C virus in human immunodeficiency virus-infected patients in New York City, United States. World J Gastroenterol. 2008;14:6689–93.
Gamage DG, Read TRH, Bradshaw CS, Hocking JS, Howley K, Chen MY, et al. Incidence of Hepatitis-C among HIV infected men who have sex with men (MSM) attending a sexual health service: a cohort study. BMC Infect Dis. 2011;11:39.
van de Laar TJW, van der Bij AK, Prins M, Bruisten SM, Brinkman K, Ruys TA, et al. Increase in HCV incidence among men who have sex with men in Amsterdam most likely caused by sexual transmission. J Infect Dis. 2007;196:230–8.
Turner J, Rider A, Imrie J, Copas A, Edwards S, Dodds J, et al. Behavioural predictors of subsequent hepatitis C diagnosis in a UK clinic sample of HIV positive men who have sex with men. Sex Transm Infect. 2006;82:298–300.
Danta M, Brown D, Bhagani S, Pybus OG, Sabin CA, Nelson M, et al. Recent epidemic of acute hepatitis C virus in HIV-positive men who have sex with men linked to high-risk sexual behaviours. AIDS. 2007;21:983–91.
Matheson A, Roxburgh A, Degenhardt L, Howard J, Down I. Drug use, dependence and mental health among gay, lesbian and bisexual people reporting regular methamphetamine use. Sydney: ACON and National Drug and Alcohol Research Centre, The University of New South Wales; 2010.
Bluthenthal RN, Kral AH, Gee L, Lorvick J, Moore L, Seal K, et al. Trends in HIV seroprevalence and risk among gay and bisexual men who inject drugs in San Francisco, 1988 to 2000. JAIDS. 2001;28:264–9.
Bolding G, Sherr L, Elford J. Use of anabolic steroids and associated health risks among gay men attending London gyms. Addiction. 2002;97:195–203.
Hunt N, Griffiths P, Southwell M, Stillwell G, Strang J. Preventing and curtailing injecting drug use: a review of opportunities for developing and delivering ‘route transition interventions’. Drug Alcohol Rev. 1999;18:441–51.
Bridge J. Route transition interventions: potential public health gains from reducing or preventing injecting. Int J Drug Policy. 2010;21:125–8.
Leonard L, DeRubeis E, Pelude L, Medd E, Birkett N, Seto J. “I inject less as I have easier access to pipes”: injecting, and sharing of crack-smoking materials, decline as safer crack-smoking resources are distributed. Int J Drug Policy. 2008;19:255–64.
Drug Misuse and Trafficking Act 1985 No 226 (NSW). Part 2, Division 1, Section 11A. http://www.legislation.nsw.gov.au/inforcepdf/1985-226.pdf?id=46cd4783-9c07-6213-ce11-fba9930ef61f. Accessed 14 August 2012.
Justice Legislation Further Amendment Act 2010. (Vic) No. 64 of 2010. http://www.legislation.vic.gov.au/. Accessed 14 August 2012.
Customs (Prohibited Imports) Amendment Regulations 2011 (No. 3) (Cth). Select Legislative Instrument 2011 No. 232. http://www.comlaw.gov.au/Details/F2011L02610. Accessed 14 August 2012.
Acknowledgments
Thank you to the men who participated in the Sydney GCPS, the community organisations who made the recruitment possible, and the state and territory health departments who funded the surveys. The National Centre in HIV Social Research and the Kirby Institute are supported by the Australian Government Department of Health and Ageing.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lea, T., Mao, L., Bath, N. et al. Injecting drug use among gay and bisexual men in Sydney: prevalence and associations with sexual risk practices and HIV and hepatitis C infection. AIDS Behav 17, 1344–1351 (2013). https://doi.org/10.1007/s10461-013-0409-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-013-0409-0