Abstract
We assessed the cost-effectiveness of including boys vs girls alone in a pre-adolescent vaccination programme against human papillomavirus (HPV) types 16 and 18 in Brazil. Using demographic, epidemiological, and cancer data from Brazil, we developed a dynamic transmission model of HPV infection between males and females. Model-projected reductions in HPV incidence under different vaccination scenarios were applied to a stochastic model of cervical carcinogenesis to project lifetime costs and benefits. We assumed vaccination prevented HPV-16 and -18 infections in individuals not previously infected, and protection was lifelong. Coverage was varied from 0-90% in both genders, and cost per-vaccinated individual was varied from I$25 to 400. At 90% coverage, vaccinating girls alone reduced cancer risk by 63%; including boys at this coverage level provided only 4% further cancer reduction. At a cost per-vaccinated individual of $50, vaccinating girls alone was <$200 per year of life saved (YLS), while including boys ranged from $810–18 650 per YLS depending on coverage. For all coverage levels, increasing coverage in girls was more effective and less costly than including boys in the vaccination programme. In a resource-constrained setting such as Brazil, our results support that the first priority in reducing cervical cancer mortality should be to vaccinate pre-adolescent girls.
Similar content being viewed by others
Main
Cervical cancer is the second most common cancer in women worldwide (Parkin and Bray, 2006), with the majority of cases and deaths occurring in low-resource countries where organised screening has not been feasible, for example, nearly 20 000 women in Brazil are predicted to develop cervical cancer over the next year (Ferlay et al, 2004). Vaccines designed to prevent infections with human papillomavirus (HPV)-16 and -18, responsible for roughly 70% of cases, provide an opportunity for primary prevention. Clinical trials of these vaccines have shown a high degree of efficacy at preventing types 16 and 18 associated infection and precancerous changes in women not previously infected with these types (Harper et al, 2006; Ault, 2007; Future II Study Group, 2007; Garland et al, 2007; Paavonen et al, 2007).
Reductions in cervical cancer mortality by pre-adolescent HPV vaccination would not be observable for many years. Mathematical models that synthesize the best available data while ensuring consistency with epidemiological observations can project outcomes beyond those reported in clinical trials, can provide insights into cost-effectiveness, and can be modified as new information becomes available (Garnett et al, 2006; Goldie et al, 2007). We recently used an empirically calibrated stochastic model of cervical cancer in a cost-effectiveness analysis of pre-adolescent vaccination of Brazilian girls, with specific attention to strategies that include screening (Goldie et al, 2007). Because HPV is sexually transmitted, vaccination of both sexes is being considered in some settings.
To assess the value of including boys in a vaccination programme, a dynamic transmission model is required, which captures not only the direct protective effects on vaccinated individuals, but also the potential indirect effects of reducing HPV transmission to their partners (Edmunds et al, 1999; Brisson and Edmunds, 2003; Garnett, 2005). Extending previous work by others (Hughes et al, 2002; Taira et al, 2004; Elbasha and Galvani, 2005; Barnabas et al, 2006; Dasbach et al, 2006; French et al, 2007), we developed a flexible dynamic model of HPV-16 and -18 sexual transmission between males and females. We linked this model to our stochastic model of cervical carcinogenesis that includes non-vaccine targeted (i.e., non-16, -18) high- and low-risk HPV types to assess the cost-effectiveness of including boys in a pre-adolescent vaccination programme in Brazil.
Materials and methods
Dynamic model
A simplified schematic of the dynamic transmission model is shown in Figure 1. It is an open-cohort, age-structured (ages 0–90 in yearly intervals) compartmental model in which females and males form sexual partnerships over time. Sexually-naive girls and boys enter the susceptible pool upon sexual initiation starting at age 12, and with each partnership, HPV-16 and -18 can be transmitted. Following first HPV infection and clearance, individuals may develop type-specific natural immunity, effectively reducing their susceptibility to future same-type infection. Women with HPV infection can develop cervical intraepithelial neoplasia, grade 1 (CIN 1) or grade 2–3 (CIN 2,3), and those with CIN 2,3 may develop invasive cancer. Males can acquire HPV infection from infected females with or without CIN.
Schematic of dynamic model for females. Females who are uninfected can acquire HPV-16 or -18 infection (at an annual rate of λ16 or λ18, respectively). Once infected, females can develop precancerous lesions (i.e., CIN 1 and CIN 2,3), and over time may develop invasive cervical cancer. Females who clear their infection or lesion develop a degree of natural immunity to that same HPV type (i.e., immune16 or immune18); future type-specific infections can be acquired at a reduced rate (e.g., λ16*(1-immune16)). History of prior infection is tracked throughout the analysis. Note: not all health states and transitions are shown. The model for males has a similar structure for HPV-16 and -18 infection only (the schematic and corresponding model equations can be found in the Supplementary information). Once vaccination is introduced, females and males enter a corresponding vaccinated state; vaccine efficacy is modelled as protection against future type-specific infection.
Input parameters for the model were estimated using primary data from longitudinal epidemiological studies and other published literature, and for some inputs, were indirectly estimated using calibration methods. Population and demographic statistics from Brazil were used to inform population size, and birth and death rates (U.S. Census Bureau, 2000; U.N. Population Division, 2004). We adapted a previously published sexual mixing algorithm (Barnabas et al, 2006) to reflect data on sexual behaviour in Brazil, such as age of sexual debut and number of sexual partners (U.S.A.I.D., 2006). Briefly, depending on age, members of the male and female cohorts belong to one of four sexual activity groups (none, low, moderate, and high), which govern the number of new sexual partners per year. Each year, type-specific HPV incidence changes according to the number of new partners, HPV prevalence in the opposite gender, and the probability of HPV transmission given a partner has HPV-16 or -18 infection. Details of model structure, input parameters and sexual mixing assumptions are provided in the Supplementary information.
A likelihood-based calibration exercise was used to identify combinations of four uncertain parameter values that produced good model fit to empirical data. These parameters included (1) transmission probability of HPV-16 per infected-susceptible partnership, (2) transmission probability of HPV-18 per infected-susceptible partnership, (3) clearance rate of HPV-16 and -18 infection, and (4) progression rate of CIN 2,3 to invasive cancer. We employed the following approach: more than 100 000 model simulations were run in the absence of vaccination or screening. For each simulation, one value for each of the four parameters was randomly selected from a uniform distribution over pre-specified plausible ranges, creating a unique natural history parameter set. Model outcomes using each parameter set were scored according to their fit with calibration targets established using epidemiological data from studies in Brazil and other South American countries. Good-fitting sets were identified based on a composite goodness-of-fit score. Details of these methods are provided in the Supplementary information.
Using the best-fitting parameter set, we projected reductions in HPV-16 and -18 incidence that would be expected over time with and without HPV vaccination of pre-adolescent girls alone vs boys and girls. We assumed vaccination occurred in girls and boys before age 12 and provided lifetime protection against all incident HPV-16 and -18 infections. Coverage rates were varied from 0 to 90% in girls and boys independently. After the epidemic achieved equilibrium post-vaccination, age-specific incidence rates of HPV-16 and -18 were generated for each vaccination scenario. The reductions in HPV incidence projected from the dynamic transmission model were then used as direct inputs to our previously described stochastic model (Goldie et al, 2007; Kim et al, 2007). The latter model differs from the dynamic transmission model in the following ways: (1) only females are represented; (2) all HPV types (both vaccine-targeted and non-targeted) are included; (3) HPV incidence is a function of age and individual-level characteristics, but does not explicitly change over time in response to sexual activity and population prevalence; (4) it is an individual-based model, which keeps track of each woman's history; and (5) it is stochastic, reflecting variability as well as uncertainty. Like the dynamic transmission model, it is empirically calibrated to epidemiological data (Goldie et al, 2007; Kim et al, 2007).
Cost-effectiveness analysis
Lifetime costs, life expectancy, and incremental cost-effectiveness ratios were estimated for including boys in a vaccination programme compared to girls alone. Estimations of costs (e.g., cancer treatment) are documented elsewhere (Goldie et al, 2007), but briefly, we included direct medical costs, nonmedical costs, and time costs. Since the price of the vaccine and cost of delivery in Brazil is uncertain, we assumed a composite cost per-vaccinated individual, which was varied from I$25 to 400; for example, for a composite cost of $25 per-vaccinated individual, we assumed three doses of vaccine at $5 each ($15), wastage of $2.25, freight and supplies of $1.31, administration of $1.50, and vaccine support and programmatic costs of $4.94 (Goldie et al, 2007). Costs are presented in 2000 international dollars, a currency that provides a means of comparing costs among countries, taking into account differences in purchasing power (World Health Organization, 2007).
Following published guidelines for economic evaluations, we adopted a societal perspective and included all costs and benefits regardless to whom they accrue and discounted future costs and life years by 3% annually (Gold et al, 1996). The performance of alternative strategies was measured using the incremental cost-effectiveness ratio, which is defined as the additional cost of a specific strategy, divided by its additional benefit compared with the next-most-expensive strategy. Strategies were excluded from the cost-effectiveness calculations if they were more costly and less effective (i.e., strongly dominated) or less costly and less cost-effective (i.e., weakly dominated) than an alternative strategy. We assessed the model's internal consistency (against data used as inputs), external consistency (against known facts about the disease), projective validity (against data sourced independently from model inputs), and convergent validity (against results from different models) (Weinstein et al, 2003).
Results
Model calibration and validity
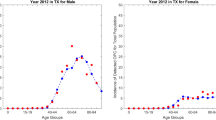
The calibrated values of the four parameters in the best-fitting parameter set, and the mean and range of values for the 10 best-fitting sets, are presented in the Supplementary information. Figure 2 shows examples of model output from the 10 sets with the best goodness-of-fit scores compared with empirical prevalence data of HPV-16 (upper panel) and -18 (lower panel) from two large epidemiological studies in South America (Franco et al, 1999; Molano et al, 2002; Clifford et al, 2005). External consistency of the model was demonstrated by producing outcomes that were within the 95% confidence intervals of independent data, including age-specific cancer incidence rates (HPV-16 and -18 associated only) (International Agency for Research on Cancer, 1976; Clifford et al, 2003a, 2003b, 2006) (Figure 3). Additional calibration results and an assessment of projective validity are provided in the Supplementary information.
Model output of age-specific prevalence of HPV-16 (upper panel) and HPV-18 (lower panel) among females compared to empirical data. Red dotted line represents model output for the best-fitting set; grey lines represent model output for the next nine best-fitting sets. Black solid lines depict the 95% confidence interval of the empirical data at each age group (Franco et al, 1999; Molano et al, 2002; Clifford et al, 2005, 2006).
Model output of age-specific incidence of cervical cancer (HPV-16 and-18 associated only) compared to empirical data. Red dotted line represents model output for the best-fitting set; grey lines represent model output for the next nine best-fitting sets. Black solid lines depict the 95% confidence interval of the empirical data at each age group (International Agency for Research on Cancer, 1976; Clifford et al, 2003a, 2003b, 2006).
Clinical benefits and cost-effectiveness of vaccination
Shown in Table 1 are the reductions in lifetime cancer risk and the cost-effectiveness ratios associated with vaccinating both boys and girls vs girls alone at different costs per-vaccinated individual ($25–400) and coverage rates (equal for both genders). In a vaccination programme for pre-adolescent girls alone, benefits were generally proportional to the level of coverage; for example, reduction in overall cancer risk was 14% with 25% coverage, and 63% with 90% coverage. When boys were added to the vaccination programme, cancer reduction was consistently higher than when covering girls alone; however, the magnitude of the incremental benefit of including boys depended on the level of coverage achieved for girls. For example, at 50% coverage of girls, reduction in lifetime risk of cancer increases from 29 to 40% when including equal coverage of boys; in contrast, at 90% coverage, reduction in cancer increases from 63 to 67% when including boys.
At a composite cost of $25 per-vaccinated individual (approximately $5 per dose), vaccinating pre-adolescent girls alone was cost-saving compared to no vaccination, at all coverage levels. When this cost increased to $50 (approximately $12 per dose), vaccination was no longer cost-saving, and the cost-effectiveness ratios varied by level of coverage; while vaccinating girls only was consistently less than $200 per year of life saved (YLS), the ratio for vaccinating both girls and boys increased from $810 per YLS to $18 650 per YLS, as coverage increased. This trend was consistent at higher costs.
Because countries may consider investments to increase vaccine coverage, we explored the tradeoffs associated with increasing coverage in girls vs including boys in a vaccination programme (Table 2). At initial coverage levels of 25 or 75% for alone, a strategy of including boys was always more costly and less effective than increasing coverage for girls; for example, when considering investments beyond 25% coverage in girls alone, a strategy of increasing their coverage to 50% provided an 8% greater reduction in cancer risk and was less costly than adding 25% coverage in boys. Even with 75% coverage in girls, increasing their coverage to 90% was more effective and less costly than adding coverage of boys up to 25, 50, or 75%.
Results of other sensitivity analyses, including varying assumptions about type-specific natural immunity, an increase in cancer caused by non-vaccine targeted HPV types, cross-protection extending to other HPV types, and waning vaccine immunity, produced findings similar to those reported in previous analyses (Goldie et al, 2007).
Discussion
The goal of our analysis is to inform discussions about how best to reduce deaths from cervical cancer in Brazil and epidemiologically similar countries. Our results suggest that for a pre-adolescent vaccination programme in which coverage of girls is high, the added value of including boys will be relatively small compared with settings in which coverage of girls is low. While there were increased health benefits for females when boys were included at any coverage level, the marginal impact on cervical cancer incidence diminished as coverage in girls increased, while total costs nearly doubled (assuming same coverage for both genders), resulting in less attractive cost-effectiveness ratios. When we comparatively assessed the impact of increasing coverage in girls to including boys in the vaccination programme, we found that even a modest increase in coverage of girls was less costly, yet more beneficial, than covering an equal percentage of boys. In other words, at any specific coverage level, a decision maker faced with the choice of trying to expand coverage in girls vs including boys should always increase coverage in girls first, all else being equal.
The Commission on Macroeconomics and Health has suggested that interventions with ratios below per capita GDP should be considered ‘very cost-effective’ (World Health Organization, 2001). For Brazil, this would imply a threshold of approximately I$ 8600 (U.S. Central Intelligence Agency, 2007). Some would argue that the real-world threshold for a new programme should be the incremental cost-effectiveness ratios of other public health interventions competing for the same resources, such as vaccines that have already been implemented. In this case, the relevant threshold ratio could be as low as $500 per YLS (Jha et al, 1998). Adopting this lower threshold would imply that the cost per-vaccinated person would need to approximate or be lower than $50 for pre-adolescent vaccination of girls to be cost-effective. Further, unless this cost is well below $50, coverage in girls is well below 50%, and coverage in girls could not be increased, then adding boys to a vaccination programme may not be cost-effective in Brazil. We acknowledge however, that cost-effectiveness is one of the many factors that influence decision-making and that there may be other considerations, such as equity, community perception, cultural preferences, and political realities that will play a larger role.
As recommended in guidelines for health economic evaluations (Gold et al, 1996), we adopted a societal perspective and considered a long time horizon that captures not only the immediate costs of vaccination, but also the future costs averted by preventing cancer in later years. While cost-effectiveness analysis provides information on ‘value for money’, it is not equivalent to providing information on the budget impact to a local decision maker. Although countries need to conduct their own financial analyses, estimating the financial resources required for a vaccination programme over the first few years can provide useful, albeit daunting, qualitative insights. For example, at a cost per-vaccinated girl of $100, vaccinating just 50% of 11-year-old girls is projected to exceed $85 million in just the first year of the programme. Adding boys at the same coverage level would double the cost. Of note, because our analysis presents cost-effectiveness results in international dollars, the relevant financial assessment would convert the tradeable portion of the intervention cost (e.g., vaccine) using the foreign exchange rate, and express all costs in local currency.
Our results associated with vaccinating girls alone were consistent with those obtained in a previous analysis we conducted in Brazil using our stochastic model of girls (Goldie et al, 2007). In particular, we found that the cost-effectiveness of HPV vaccination was most influenced by the vaccine price and cost of delivering adolescent vaccination. Although dynamic transmission models of HPV infection are increasingly being developed to explore the population-level impact of an HPV vaccine, to date, there are few that evaluate the cost-effectiveness of vaccinating both boys and girls within vaccination programmes (Taira et al, 2004; Dasbach et al, 2006; Elbasha et al, 2007; Newall et al, 2007), and none pertaining to low-resource settings. These studies, conducted in the context of current screening in the United States, have drawn similar conclusions that vaccinating 12-year-old girls is an attractive strategy. However, while Taira et al (2004) found that including boys in a vaccination programme costs nearly $450 000 per quality-adjusted life years (QALY) gained, Elbasha et al (2007) concluded that vaccinating both boys and girls, with catch-up programmes up to age 24 for both sexes, costs $45 100 per QALY. Although Elbasha et al (2007) capture the vaccine benefits of reducing HPV-6 and -11 related sequelae, they do not incorporate the impact of the vaccine on overall cancer incidence associated with all HPV types. Similar to Taira et al (2004), we employed two distinct types of models to address this issue and capitalise on the strengths of each. In the dynamic model, we reflected the infectious transmission of HPV-16 and -18 among sexually active males and females to capture herd immunity effects, and in the stochastic model, we translated the benefits of a vaccine targeting two types of HPV to overall cancer incidence associated with all high-risk HPV types.
As with all modelling approaches there are limitations to our analysis that should be noted. First, like others (Hughes et al, 2002; Barnabas et al, 2006; Burchell et al, 2006), we indirectly estimated HPV transmission probabilities per infected-susceptible partnership. Although similar to the calibrated estimates of transmission per coital act by Burchell et al (2006), our calibrated values of transmission probability per infected-susceptible partnership for HPV-16 and -18 were lower than those estimated from other studies (Hughes et al, 2002; Barnabas et al, 2006); however, we modelled a different population with different HPV prevalence and sexual behaviours and allowed other uncertain variables, such as HPV clearance and CIN 2,3 progression to cancer, to simultaneously vary in the fitting process, as well. As better data become available on age- and gender-specific transmission, it will be important to reassess these estimates.
As we await data on vaccine efficacy in boys, we made an assumption that the vaccine was as efficacious in reducing HPV-16 and -18 incidence among boys as it is for girls. Even under such generous assumptions, we found that investing in increased coverage of girls was far more favourable than including boys in a vaccination programme. We did not, however, consider the potential benefits of the quadrivalent HPV vaccine in preventing HPV-6 and -11 associated genital warts, as our analysis was explicitly focused on reducing cervical cancer mortality; any positive externalities that are not included in the analysis would improve the cost-effectiveness of the vaccine in the overall population. We did not include other cancers associated with HPV-16 and -18, as data in Brazil are limited, and also because their natural histories are not well-elucidated to model over decades. Detailed sexual behaviour data are limited. Not only is there severe under-reporting and misreporting of sexual behaviour, but there are also significant time trends that may be occurring in developing countries with respect to age of sexual initiation and number of partners that can impact overall incidence of HPV. To the extent that childhood exposure to HPV (e.g., from sexual abuse or mother-to-child transmission), and in particular HPV-16 and -18, is underestimated, we may be overestimating the protective effects of the vaccine. We did not model bisexual or homosexual partnerships, nor did we include risk factors that may be changing over time, such as smoking (Ho et al, 1998; Munoz et al, 2006).
We assumed individuals had an equal chance of getting vaccinated, but in reality, uptake may be lower in settings with less access to adolescents, such as rural areas and where children are not in school. It will therefore be important to monitor differential uptake and post-vaccination behaviour. Finally, as we have previously reported, potentially influential uncertainties such as the duration of vaccine efficacy, magnitude of herd immunity, cross protection, interactions between HPV types and natural history of multiple infections all represent data gaps; modelled estimates will improve as better information becomes available.
In light of the range of uncertainties and the unavoidable limitations inherent in modelling methods, we present our findings as exploratory and aim to provide qualitative insight into decisions that countries will be facing in the coming years regarding HPV vaccine implementation. On the basis of the most current epidemiological data, the results of this analysis suggest that the benefits of including boys in an HPV vaccination programme depend on the level of coverage achievable for girls, and in particular, the added benefit on cancer reduction is relatively small provided coverage of girls is greater than 75%. Moreover, even at this coverage level, expanding coverage in girls is more cost-effective than adding boys to the vaccination programme. In a resource-constrained setting such as Brazil, our results support that the first priority in reducing cervical cancer mortality should be to vaccinate pre-adolescent girls.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Ault KA (2007) Effect of prophylactic human papillomavirus L1 virus-like-particle vaccine on risk of cervical intraepithelial neoplasia grade 2, grade 3, and adenocarcinoma in situ: a combined analysis of four randomised clinical trials. Lancet 369: 1861–1868
Barnabas RV, Laukkanen P, Koskela P, Kontula O, Lehtinen M, Garnett GP (2006) Epidemiology of HPV 16 and cervical cancer in Finland and the potential impact of vaccination: mathematical modelling analyses. PLoS Med 3: e138
Brisson M, Edmunds WJ (2003) Economic evaluation of vaccination programs: the impact of herd-immunity. Med Decis Making 23: 76–82
Burchell AN, Richardson H, Mahmud SM, Trottier H, Tellier PP, Hanley J, Coutlee F, Franco EL (2006) Modeling the sexual transmissibility of human papillomavirus infection using stochastic computer simulation and empirical data from a cohort study of young women in Montreal, Canada. Am J Epidemiol 163: 534–543
Clifford G, Franceschi S, Diaz M, Munoz N, Villa LL (2006) Chapter 3: HPV type-distribution in women with and without cervical neoplastic diseases. Vaccine 24(Suppl 3): S26–S34
Clifford GM, Gallus S, Herrero R, Munoz N, Snijders PJ, Vaccarella S, Anh PT, Ferreccio C, Hieu NT, Matos E, Molano M, Rajkumar R, Ronco G, de Sanjose S, Shin HR, Sukvirach S, Thomas JO, Tunsakul S, Meijer CJ, Franceschi S (2005) Worldwide distribution of human papillomavirus types in cytologically normal women in the international agency for research on cancer HPV prevalence surveys: a pooled analysis. Lancet 366: 991–998
Clifford GM, Smith JS, Aguado T, Franceschi S (2003a) Comparison of HPV type distribution in high-grade cervical lesions and cervical cancer: a meta-analysis. Br J Cancer 89: 101–105
Clifford GM, Smith JS, Plummer M, Munoz N, Franceschi S (2003b) Human papillomavirus types in invasive cervical cancer worldwide: a meta-analysis. Br J Cancer 88: 63–73
Dasbach EJ, Elbasha EH, Insinga RP (2006) Mathematical models for predicting the epidemiologic and economic impact of vaccination against human papillomavirus infection and disease. Epidemiol Rev 28: 88–100
Edmunds WJ, Medley GF, Nokes DJ (1999) Evaluating the cost-effectiveness of vaccination programmes: a dynamic perspective. Stat Med 18: 3263–3282
Elbasha EH, Galvani AP (2005) Vaccination against multiple HPV types. Math Biosci 197: 88–117
Elbasha EH, Dasbach EJ, Insinga RP (2007) Model for assessing human papillomavirus vaccination strategies. Emerg Infect Dis 13: 28–41
Ferlay J, Bray F, Pisani P, Parkin DM (2004) Globocan 2002: Cancer Incidence, Mortality, and Prevalence Worldwide. Lyon: IARC Press
Franco EL, Villa LL, Sobrinho JP, Prado JM, Rousseau MC, Desy M, Rohan TE (1999) Epidemiology of acquisition and clearance of cervical human papillomavirus infection in women from a high-risk area for cervical cancer. J Infect Dis 180: 1415–1423
French KM, Barnabas RV, Lehtinen M, Kontula O, Pukkala E, Dillner J, Garnett GP (2007) Strategies for the introduction of human papillomavirus vaccination: modelling the optimum age- and sex-specific pattern of vaccination in Finland. Br J Cancer 96: 514–518
Future II Study Group (2007) Quadrivalent vaccine against human papillomavirus to prevent high-grade cervical lesions. N Engl J Med 356: 1915–1927
Garland SM, Hernandez-Avila M, Wheeler CM, Perez G, Harper DM, Leodolter S, Tang GW, Ferris DG, Steben M, Bryan J, Taddeo FJ, Railkar R, Esser MT, Sings HL, Nelson M, Boslego J, Sattler C, Barr E, Koutsky LA (2007) Quadrivalent vaccine against human papillomavirus to prevent anogenital diseases. N Engl J Med 356: 1928–1943
Garnett GP (2005) Role of herd immunity in determining the effect of vaccines against sexually transmitted disease. J Infect Dis 191(Suppl 1): S97–S106
Garnett GP, Kim JJ, French K, Goldie SJ (2006) Chapter 21: modelling the impact of HPV vaccines on cervical cancer and screening programmes. Vaccine 24(Suppl 3): S178–S186
Gold MR, Siegel JE, Russel LB, Weinstein MC (1996) Cost-Effectiveness in Health and Medicine. New York: Oxford University Press
Goldie SJ, Kim JJ, Kobus KE, Goldhaber-Fiebert JD, Salomon JA, O'Shea MKH, Bosch FX, De Sanjose S, Franco EL (2007) Cost-effectivness of HPV 16,18 vaccination in Brazil. Vaccine 25: 6257–6270
Harper DM, Franco EL, Wheeler CM, Moscicki AB, Romanowski B, Roteli-Martins CM, Jenkins D, Schuind A, Costa Clemens SA, Dubin G (2006) Sustained efficacy up to 4.5 years of a bivalent L1 virus-like particle vaccine against human papillomavirus types 16 and 18: follow-up from a randomised control trial. Lancet 367: 1247–1255
Ho GY, Kadish AS, Burk RD, Basu J, Palan PR, Mikhail M, Romney SL (1998) HPV 16 and cigarette smoking as risk factors for high-grade cervical intra-epithelial neoplasia. Int J Cancer 78: 281–285
Hughes JP, Garnett GP, Koutsky L (2002) The theoretical population-level impact of a prophylactic human papilloma virus vaccine. Epidemiology 13: 631–639
International Agency for Research on Cancer (1976) Cancer Incidence in Five Continents, vol.3. Vol.3. IARC Scientific Publications No. 15 Lyon: IARC Press
Jha P, Bangoura O, Ranson K (1998) The cost-effectiveness of forty health interventions in Guinea. Health Policy Plan 13: 249–262
Kim JJ, Kuntz KM, Stout NK, Mahmud S, Villa LL, Franco EL, Goldie SJ (2007) Multiparameter calibration of a natural history model of cervical cancer. Am J Epidemiol 166: 137–150
Molano M, Posso H, Weiderpass E, van den Brule AJ, Ronderos M, Franceschi S, Meijer CJ, Arslan A, Munoz N (2002) Prevalence and determinants of HPV infection among Colombian women with normal cytology. Br J Cancer 87: 324–333
Munoz N, Castellsague X, de Gonzalez AB, Gissmann L (2006) Chapter 1: HPV in the etiology of human cancer. Vaccine 24S3: S1–S10
Newall AT, Beutels P, Wood JG, Edmunds WJ, Macintyre CR (2007) Cost-effectiveness analyses of human papillomavirus vaccination. Lancet Infect Dis 7: 289–296
Paavonen J, Jenkins D, Bosch FX, Naud P, Salmeron J, Wheeler CM, Chow SN, Apter DL, Kitchener HC, Castellsague X, de Carvalho NS, Skinner SR, Harper DM, Hedrick JA, Jaisamrarn U, Limson GA, Dionne M, Quint W, Spiessens B, Peeters P, Struyf F, Wieting SL, Lehtinen MO, Dubin G (2007) Efficacy of a prophylactic adjuvanted bivalent L1 virus-like-particle vaccine against infection with human papillomavirus types 16 and 18 in young women: an interim analysis of a phase III double-blind, randomised controlled trial. Lancet 369: 2161–2170
Parkin DM, Bray F (2006) Chapter 2: The burden of HPV-related cancers. Vaccine 24(Suppl 3): S11–S25
Taira AV, Neukermans CP, Sanders GD (2004) Evaluating human papillomavirus vaccination programs. Emerg Infect Dis 10: 1915–1923
U.N. Population Division (2004) World Population Prospects: The 2004 Revision Population Database. http://esa.un.org/unpp/ Last accessed on January 19, 2007
U.S. Census Bureau (2000) Population Estimates Program, Population Division: Washington, DC. http://www.census.gov/ipc/www/idb/index.html: Last accessed on September 24, 2007
U.S. Central Intelligence Agency (2007) The World Factbook. https://www.cia.gov/library/publications/the-world-factbook/geos/br.html: Last accessed on September 24, 2007
U.S.A.I.D. (2006) Demographic and Health Surveys. http://www.measuredhs.com/ Last accessed on January 19, 2007
Weinstein MC, O'Brien B, Hornberger J, Jackson J, Johannesson M, McCabe C, Luce BR (2003) Principles of good practice for decision analytic modeling in health-care evaluation: report of the ISPOR task force on good research practices – modeling studies. Value Health 6: 9–17
World Health Organization (2001) Investing in Health for Economic Development. Report of the Commission on Macroeconomics and Health. Geneva: World Health Organization
World Health Organization (2007) WHO CHOICE (Choosing Interventions That Are Cost-Effective). http://www.who.int/choice/en/ Last accessed on January 19, 2007
Acknowledgements
This study was supported in part by grants from the National Cancer Institute (R01 CA93435) and from the Bill and Melinda Gates Foundation (30505). We gratefully acknowledge the early contributions of Megan Murray and helpful reviews from Angela Raffle and Ruanne Barnabas.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on British Journal of Cancer website (http://www.nature.com/bjc)
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Kim, J., Andres-Beck, B. & Goldie, S. The value of including boys in an HPV vaccination programme: a cost-effectiveness analysis in a low-resource setting. Br J Cancer 97, 1322–1328 (2007). https://doi.org/10.1038/sj.bjc.6604023
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6604023
Keywords
This article is cited by
-
A Dynamic Model to Assess Human Papillomavirus Vaccination Strategies in a Heterosexual Population Combined with Men Who have Sex with Men
Bulletin of Mathematical Biology (2021)
-
Assessing the cost-effectiveness of HPV vaccination strategies for adolescent girls and boys in the UK
BMC Infectious Diseases (2019)
-
Operations research in global health: a scoping review with a focus on the themes of health equity and impact
Health Research Policy and Systems (2017)
-
Challenges in Cost-Effectiveness Analysis Modelling of HPV Vaccines in Low- and Middle-Income Countries: A Systematic Review and Practice Recommendations
PharmacoEconomics (2017)
-
Human Papilloma Virus Infections in Men: Focus on Vaccination and Treatment Options
Current Treatment Options in Infectious Diseases (2017)