Abstract
Anal human papillomavirus (HPV) infection, which is linked to anal warts and anal cancer, is common among men who have sex with men (MSM), especially among those HIV positives. MSM aged 18 years or older were recruited from mainland China. Blood and anal cytologic samples were collected for HIV-1 serological test and HPV genotyping. A total of 889 eligible participations were included. The genotyping results of HPV were available for 822 participants (92.46%), 65.32% of which were positive for the targeted 37 HPV types. Prevalence of infection with any type of HPV was higher among HIV-infected participants (82.69%) as compared to HIV-uninfected participants (62.81%) (p < 0.01). HPV06 (15.45%), HPV18(13.50%), HPV16 (11.44%) and HPV11 (10.71%) were the most frequent types identified in the study population. Ever had paid sex with man was found to be independent predictor for HPV positivity with an adjusted odds ratios (OR) of 2.34 (1.16–4.74). Anal HPV positivity was observed to be independently associated with HIV infection with an adjusted OR of 3.03 (1.76–5.21) in the study population. In conclusion, the prevalence of anal HPV infection was observed to be common among MSM from mainland China and it was significantly associated with the status of HIV infection.
Similar content being viewed by others
Introduction
Anal infection with human papillomavirus (HPV) is extremely common in men who have sex with men (MSM)1,2,3. Although most HPV infections are transient and clinically unapparent, close attention has been paid to HPV because of its causal link to certain cancers. Besides the established association between high-risk HPV infection and cervical cancer, persistent HPV infection has also been suggested to be an important risk factor for the development of several other cancers, such as laryngeal cancer, esophageal cancer and anal cancer4,5,6. Our previous study showed that 62.10% of the MSMs from Beijing and Tianjin cities had been infected with HPV, including several oncogenic HPV types such as 16, 18, 31, 33, 35, 45, 52 and 587. In addition, previous studies show that nearly all of the HIV-positive MSM were infected with HPV, which was approximately 1.5 times higher than HIV-negative MSM7,8. A recent systematic review and meta-analysis which included 21 studies of HIV-positive MSM reported a summary prevalence estimate of HPV infection any type to be 92.6% (90.8–94.5)9. Epidemiologic assessment indicated that behavioral factors might play roles in the prevalence, incidence and persistence of anal HPV infection, such as the mounts of sex partners, unprotected anal sex and cigarette smoking7,8,10.
In recent years, the prevalence of HIV/AIDS and other sexually transmitted diseases (STDs) in China have been rapidly rising among MSM, which draws great concern of the public health fields11,12. Stigma and discrimination related to homosexual activities and HIV/STD infection have been the major barriers to MSM seeking health services13. In China, homosexuality is still regarded as deviation from mainstream society despite of an increasing acceptance of MSM in general society. Stigma and social pressure for MSM in China were reported to mainly arise from their families to get married and have children to protect family reputation and lineage. This might increase the risk of HIV spread from the high-risk population to general population. The study by Zhang Lei and colleagues indicated HIV prevalence in MSM in China increased from 1.77% (1.26–2.57) in 2000, to 5.98% (4.43–8.18) in 2010, with a national incidence of 0.98 (0.70–1.25) per 100 person-years in 201014. Therefore, the prevalence of anal HPV infection and its association with HIV among this high-risk population should be more widely addressed in China. It is important to examine how empirical HPV findings in Chinese MSM relate to other international studies. Based on our previous studies conducted in Beijing and Tianjin, the objectives of this cross-sectional study were investigating the status of anal HPV infection and HIV infection among MSM from other cities in China and identifying the most prevalent HPV genotypes.
Results
Subject recruitment and characteristics
In total, 889 eligible participations were interviewed and signed the informed consents, 289 from Chengdu, 300 from Xi’an and 300 from Taiyuan, respectively. Blood sample and anal swab were successfully collected from each of them. As shown in Table 1, major characteristics of the study participants were evaluated by site. Nearly half of them were younger than 30 years (47.25%), 70.53% reported homosexual tendency, 10.02% reported a history of genital wart and 11.02% reported other STDs history other than genital wart and HIV. Laboratory data suggested a prevalence of 12.26% of HIV seropositivity among the study population.
Anal HPV type distribution
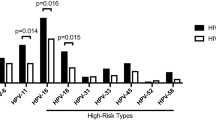
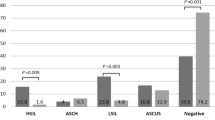
As shown in Supplementary Table S1 and Table 2, the genotyping results of HPV were available for 822 participants (92.46% of all), 65.32% of them were positive for at least one of the targeted 37 HPV types. Prevalence of infection with any type of HPV was higher among HIV-infected participants (82.69%), as compared to HIV-uninfected participants (62.81%) (p < 0.01).Among HPV positives, 41.53% (223/537) of them were infected with multiple types. Among HIV-positived participants, 17.31% had none HPV subtypes detected, 34.62% were positive for only one type and 48.08% were detected with two or more types. HPV06 (15.45%), HPV18 (13.50%), HPV16 (11.44%) and HPV11 (10.71%) were found to be the most frequently identified types. The prevalence of HPV types of 56, 82, 52, 39, 68, 51, 31, 66, 45, 33, 55, 83, 6, 61, 40 and 44 were found to be significantly higher among HIV-infected compared to uninfected participants. In addition, the distribution pattern of the genotypes was found to be various among the study sites (Supplementary Table S1).
Risk factors for anal HPV infection
The associations of anal HPV infection with potential risk factors were assessed by logistic regression analysis as shown in Table 3. Covariates with P < 0.1 in univariate models were adjusted for in a multiple logistic regression model. Ever had paid sex with man in the past year was found to be significantly related to HPV seropositivity with an adjusted OR of 2.34 (1.16–4.74).
Risk factors for HIV infection
As shown in Table 4, condom use during insertive anal sex in the past 6 months, ever found sexual partners in gay venues and anal HPV infection were significantly associated with HIV seropositivity in univariate analyses. The variables were included multiple logistic regression analysis with P < 0.1 in univariate models. Anal HPV statuses were significantly associated with HIV seropositivity with an adjusted OR of 3.03 (1.76–5.21).
The association between HIV seropositivity and anal HPV infection
As shown in Table 5, we analyzed the association between HIV status and anal HPV infection according to HPV oncogenic type and the number of co-infected HPV types. There are 73 and 346 subjects were infected with at least one High-risk subtypes among the HIV-positive and HIV-negative groups, respectively. The results showed both low-risk and high-risk HPV infection were found to be significantly related to HIV seropositivity. There was a significant association between HPV multiplicity and the prevalence of HIV.
Discussion
The present study demonstrated a high prevalence of anal HPV infection among MSM from three cities of China. The prevalence of anal HPV infection was much common among HIV-infected MSM (82.69%) than HIV negatives (62.81%). HPV18 and 16 were most frequently identified high-risk types and HPV06 and 11 were most frequently identified low-risk types, respectively. The prevalence of HPV genotypes was found might to be varied between the study sites. Additionally, the prevalence of anal HPV infection was found to be related to the status of HIV infection, which is consistent with our findings and the evidence from other regions7,8,15,16,17. The definition of High-risk HPV types was mainly according to the manufacturer’s instructions. Meanwhile, we defined the debatable High-risk HPV types by the previous studies18,19.
Although the prevalence of anal HPV infection among HIV-positive MSM from mainland China was 82.69%, it was slightly lower than those previous studies reported from HIV-positive MSM in the Canada (97.90%)20 and was significant higher than a Dutch gay-cohort study reported 65.00%21. Moreover, our result of the anal HPV infection prevalence among HIV-positive MSM was similar as a study from Thailand (85%)17. This discrepancy might be partly due to mode of life, variation in viral clearance and infection incubation time. For HIV-negative MSM, previous studies from the United States and Latin America showed the overall anal HPV prevalence was ranging from 42% to 66%2,3,22,23, which were comparable with our 62.81% anal HPV prevalence.
HPV06 (15.45%), HPV18 (13.50%), HPV16 (11.44%) and HPV11 (10.71%) were found to be the most frequently identified types among study population. But a different type distribution was observed by HIV status, the prevalence of several HPV types was significantly higher among HIV positives than among negatives. It is considered that immunosuppression from HIV infection not only increases risk of acquisition of new HPV infections, but also HPV infection persistence and reactivation of latent infections. The HPV types of 18 and 16 were the most common high-risk HPV types identified in both HIV-positive and HIV-negative MSM in our study. These data were consistent with our previous studies7. However, as compared to the study from Thailand17, the HPV types of 16 was the most common high-risk HPV types in both HIV-positive and HIV-negative MSM and the HPV18 was less common than HPV06. Our results suggest that the most frequently distributed HPV types among Chinese MSM could be covered by the current commercial HPV vaccines, which provides flexibility for HPV vaccination among this high risk population to prevent HPV infection and related diseases. Different from prior study24, in our analysis, former smokers or current smoking was not associated with a statistically significantly elevated risk of any HPV infection. Possibly due to the immunomodulatory properties only could be observed among individuals who are actively and seriously exposed to cigarette smoke.
In association analysis, we found the risk of anal HPV infection was not related to condom use during insertive anal sex in the past 6 months. There are mixed data on whether condoms decrease the incidence of HPV infection. To some extent, this might also influenced by the reason that we did not distinguish condom use during insertive anal sex or receptive anal sex. Several other studies did not find a relation between them either, perhaps because not all the condoms could effectively cover all the exposed skin susceptible to infection25,26.
In our present study, the subjects HPV infection status were grouped into four subgroups: negative for any type, positive only for high-risk, positive only for low-risk HPV and positive for both. Our results indicated that low-risk and high-risk HPV were associated with increased HIV seropositivity and the association for the high-risk HPV was higher. Previous study also demonstrates that anal HPV infection in MSM is associated with HIV acquisition24,27,28. Moreover a recent systemic review and meta-analysis included 6567 participants suggests that HPV-infected individuals have twice the risk of acquiring HIV29. However, the mechanisms are not yet clear. Several hypotheses may explain the reason HPV-infected individuals are more susceptibility of to HIV, including lesions infected HPV may be more friable and susceptible to disruption of mucosal, which may promote HIV entry and replication30,31. Further studies are warranted to clarify the underlying mechanisms for the different HPV type distribution between HIV negatives and positives.
Our study has several limitations. First, the cross-sectional nature of the study precluded us from determining the causal direction of significant associations between anal HPV infection and HIV seropositivity. Second, over reported or underreported sexual behaviors could not be completely excluded in the study, which may have introduced some misclassification of exposure bias into our estimates. Third, study results may have limited generalizability because participants were only recruited from3 cities and all of the cities were well-developed metropolitan in China. Fourth, it should be kept in mind that HPV infected cells might not be collected successfully using the current sampling method and accuracy of the test results might also be influenced by the quality of the samples. Fifth, in our study, not all the potential risk or protected sexual behavior factors were collected. For example, we did not distinguish condom use during insertive anal sex or receptive anal sex. Nonetheless, our study raises serious concern for HPV infection in MSM in China and demonstrates the importance to control HPV/HIV co-infection.
In conclusion, high prevalence of anal HPV infection was observed among MSM from mainland China. Anal HPV infection was identified to be significantly associated with HIV seropositivity. Moreover, with respect to the high prevalence of HPV/HIV co-infection in MSM, studies on anal and cervical HPV diseases in women should be done to gradually extend our observations seen here among men. With the US FDA approval of the HPV prophylactic vaccine, immunization in HPV-unexposed individuals may have the potential to reduce the risk of HPV and HIV acquisition as well. Therefore, quicken up introduction of vaccines to China market might reduce the incidence HPV and HIV to some extent. And above all, improving behavior intervention and health care in the high risk population should be paid more attention in China.
Materials and Methods
Ethic statement
The study was approved by the Ethics Committees of the Institute of Pathogen Biology, Chinese Academy of Medical Sciences & Peking Union Medical College. Written informed consent was obtained from each study participant before the interview and testing. All methods were carried out according to the approved guidelines set by The Institute of Pathogen Biology, Chinese Academy of Medical Sciences & Peking Union Medical College.
Study site and participants
We performed a cross-sectional study of HPV prevalence using anal swab specimens among HIV-infected and uninfected MSM. Study participants were recruited from 3 cities (Xi’an, Chengdu and Taiyuan) between March 2012 and December 2013, through local nongovernment organizations (Xi’an Tongkang Volunteers Workstation, Chengdu Yongle Volunteers Workstation and Taiyuan kangtong Volunteers Workstation). Multiple methods were used for recruitment including website advertisement, the community, STD clinics and voluntary HIV counseling and testing (VCT) clinics. Eligibility criteria were: (1) male and at least 18 years old, (2) self-reported ever had sex with men in the nearly past years, (3) willingness to provide blood samples for HIV and anal swab specimens to test HPV infection and genotypes and (4) able and willing to provide written informed consent.
Data collection
Data were collected using a questionnaire administered by trained interviewers in a private room. Each study participant was assigned a unique code that was used to link the questionnaire. Data were collected, including self-reported sociodemographic characteristics (e.g., age, income, ethnicity, education, employment and marriage status, smoking habits), sexual behaviors in the past 6 months, knowledge on HPV and HPV vaccine and the acceptance of the HPV vaccine. Clinical physical examination was performed to detect any genital and anal ulcers and warts. The nature of ulcers and discharges suggestive of sexually transmitted infections (STIs) were described in detail by trained physicians blinded to questionnaire data.
Sample collection and laboratory tests
The sample collection and physical examination were performed by trained and experienced physicians. Blood samples were collected for test of HIV serology. The HIV infection status was determined by an enzyme immunoassay (Wantai Biological Medicine Company, Beijing, China). And positive tests were confirmed by HIV-1/2 Western blot assay (HIV Blot 2.2 WB; Gene labs Diagnostics, Singapore). Trained health workers at each site collected anal samples by rotating saline water moistened nylon flocked swab in the anal canal for about 2 minutes. The swab was then kept in 3 mL of sample transport medium for Hybribio 37 HPV GenoArray Diagnostic Kit (Chaozhou Hybribio Limited Corporation, Guangzhou, China). Hybribio 37 HPV GenoArray Diagnostic Kit Test is based on a flow-through hybridization and gene-chip method. The low-density gene chip was pre-fixed with 37 type-specific oligonucleotides and the genotype was analyzed using HybriMax (Chaozhou Hybribio Limited Corporation). The results were then evaluated by a colorimetric change on the chip under direct visualization. Blue–purple spots were recognized as HPV positive. This testing kit can detect 37 common types of HPV, including 23 oncogenic (16, 18, 26, 31, 33, 35,39, 45, 51, 52, 56, 58, 59, 66, 68, 82,83,53, 55, 34, 57, 69 and 71) and 14 non-oncogenic types (06, 11, 40, 42, 44, 54,61, 67, 70, 72, 73, 82 and 84)18,19. Study participants with genotyping positive for any HPV type were determined to be currently infected with HPV.
Statistical analysis
Data for questionnaire responses, physical examinations and laboratory tests were entered independently by two study staff and verified with EpiData software (EpiData 3.1 for Windows, The EpiData Association Odense, Denmark). After cleaning, the data were then converted and analyzed using Statistical Analysis System (SAS 9.12 for Windows; SAS Institute Inc., NC, USA).
Descriptive analyses were performed to compare socio-demographic characteristics and sexual and drug use behaviors between HIV-infected and uninfected participants. Pearson’s chi-square test and Student’s t-test were used to compare differences between HIV-infected and uninfected participants for categorical and continuous variables, respectively.
Unconditional logistic regression models were used to evaluate the association between each variable and anal HPV infection. Multivariable logistic regression was employed to determine predictors of anal HPV infection. All variables with p-values < 0.1 in univariate analyses were entered into the multivariate logistic model. Crude odds ratios (OR) and adjusted odds ratios (adjusted OR) were calculated, as appropriate along with 95% confidence intervals (CI).
Additional Information
How to cite this article: Li, X. et al. Anal HPV/HIV co-infection among Men Who Have Sex with Men: a cross-sectional survey from three cities in China. Sci. Rep. 6, 21368; doi: 10.1038/srep21368 (2016).
References
Kreuter, A. et al. Clinical spectrum and virologic characteristics of anal intraepithelial neoplasia in HIV infection. J. Am. Acad. Dermatol. 52, 603–608 (2005).
Critchlow, C. W. et al. Effect of HIV infection on the natural history of anal human papillomavirus infection. AIDS 12, 1177–1184 (1998).
Palefsky, J. M., Holly, E. A., Ralston, M. L. & Jay, N. Prevalence and risk factors for human papillomavirus infection of the anal canal in human immunodeficiency virus (HIV)-positive and HIV-negative homosexual men. J. Infect. Dis. 177, 361–367 (1998).
Palefsky, J. M. et al. Detection of human papillomavirus DNA in anal intraepithelial neoplasia and anal cancer. Cancer Res. 51, 1014–1019 (1991).
Li, X. et al. Human papillomavirus infection and laryngeal cancer risk: a systematic review and meta-analysis. J. Infect. Dis. 207, 479–488 (2013).
Li, X. et al. Systematic review with meta-analysis: the association between human papillomavirus infection and oesophageal cancer. Aliment. Pharmacol. Ther. 39, 270–281 (2014).
Gao, L. et al. Anal HPV infection in HIV-positive men who have sex with men from China. Pols One 5, e15256 (2010).
Hu, Y. et al. Anal human papillomavirus infection among HIV-infected and uninfected men who have sex with men in Beijing, China. J. Acquir. Immune. Defic. Syndr. 64, 103–114 (2013).
Machalek, D. A. et al. Anal human papillomavirus infection and associated neoplastic lesions in men who have sex with men: a systematic review and meta-analysis. Lancet Oncol. 13, 487–500 (2012).
Nyitray, A. G. et al. Six-month incidence, persistence and factors associated with persistence of anal human papillomavirus in men: the HPV in men study. J. Infect. Dis. 204, 1711–1722 (2011).
Gao, L., Zhang, L. & Jin, Q. Meta-analysis: prevalence of HIV infection and syphilis among MSM in China. Sex Transm Infect. 85, 354–358 (2009).
Zhou, Y. et al. Prevalence of HIV and syphilis infection among men who have sex with men in China: a meta-analysis. Biomed. Res. Int. 2014, 620431 (2014).
Liu, J. X. & Choi, K. Experiences of social discrimination among men who have sex with men in Shanghai, China. AIDS Behav. 10, S25–S33 (2006).
Zhang, L. et al. HIV prevalence in China: integration of surveillance data and a systematic review. Lancet Infect Dis. 13, 955–963 (2013).
Poggio, J. L. Premalignant lesions of the anal canal and squamous cell carcinoma of the anal canal. Clin. Colon. Rectal. Surg. 24, 177–192 (2011).
Nyitray, A. G. et al. Age-specific prevalence of and risk factors for anal human papillomavirus (HPV) among men who have sex with women and men who have sex with men: the HPV in men (HIM) study. J. Infect. Dis. 203, 49–57 (2011).
Phanuphak, N. et al. Anal human papillomavirus infection among Thai men who have sex with men with and without HIV infection: prevalence, incidence and persistence. J. Acquir. Immune. Defic. Syndr. 63, 472–479 (2013).
Pei, F. et al. Human papillomavirus infection in nasal polyps in a Chinese population. J .Gen. Virol. 92, 1795–1799 (2011).
Zhu, X. et al. Carcinogenic ability quantification of human papilloma virus subtypes in eastern China. J .Gen. Virol. 87, 2106–2113 (2015).
de Pokomandy, A. et al. Prevalence, clearance and incidence of anal human papillomavirus infection in HIV-infected men: the HIPVIRG cohort study. J. Infect. Dis. 199, 965–973 (2009).
Auvert, B. et al. Association of oncogenic and nononcogenic human papillomavirus with HIV incidence. J. Acquir. Immune. Defic. Syndr. 53, 111–116 (2010).
Chin-Hong, P. V. et al. Age-Specific prevalence of anal human papillomavirus infection in HIV-negative sexually active men who have sex with men: the EXPLORE study. J. Infect. Dis. 190, 2070–2076 (2004).
Goldstone, S. et al. Prevalence of and risk factors for human papillomavirus (HPV) infection among HIV-seronegative men who have sex with men. J. Infect. Dis. 203, 66–74 (2011).
Schabath, M. B. et al. Smoking and human papillomavirus (HPV) infection in the HPV in Men (HIM) study. Cancer Epidemiol Biomarkers Prev. 21, 102–110 (2012).
Vaccarella, S. et al. Sexual behavior, condom use and human papillomavirus: pooled analysis of the IARC human papillomavirus prevalence surveys. Cancer Epidemiol Biomarkers Prev. 15, 326–333 (2006).
Holmes, K. K., Levine, R. & Weaver, M. Effectiveness of condoms in preventing sexually transmitted infections. Bull World Health Organ. 82, 454–461 (2004).
Houlihan, C. F. et al. Human papillomavirus infection and increased risk of HIV acquisition. A systematic review and meta-analysis. AIDS 26, 2211–2222 (2012).
Chin-Hong, P. V. et al. Anal human papillomavirus infection is associated with HIV acquisition in men who have sex with men. AIDS 23, 1135–1142 (2009).
Lissouba, P., Van de Perre, P. & Auvert, B. Association of genital human papillomavirus infection with HIV acquisition: a systematic review and meta-analysis. Sex Transm Infect. 89, 350–356 (2013).
Chin-Hong, P. V. & Palefsky, J. M. Natural history and clinical management of anal human papillomavirus disease in men and women infected with human immunodeficiency virus. Clin. Infect. Dis. 35, 1127–1134 (2002).
Jay, N. et al. Colposcopic appearance of anal squamous intraepithelial lesions: relationship to histopathology. Dis. Colon. Rectum. 40, 919–928 (1997).
Acknowledgements
We thank volunteers from Xi’an Tongkang Volunteers Workstation, Chengdu Yongle Volunteers Workstation and Taiyuan kangtong Volunteers Workgroup for their great efforts on enrollment of study participants. The work was supported by MSD China Holding Co., Ltd (Grant No: IISP ID 38859).
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: L.G., Q.J. and X.L. Performed the experiments: X.L., M.L., Z.L., H.X., X.Z. and B.F. Analyzed the data: L.G., Q.J., X.L., M.L. and Y.Y. Contributed reagents/materials/analysis tools: Q.J. and X.L. Wrote the paper: X.L. and L.G.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Li, X., Li, M., Yang, Y. et al. Anal HPV/HIV co-infection among Men Who Have Sex with Men: a cross-sectional survey from three cities in China. Sci Rep 6, 21368 (2016). https://doi.org/10.1038/srep21368
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep21368
This article is cited by
-
Anal human papillomavirus infection and its relationship with abnormal anal cytology among MSM with or without HIV infection in Japan
Scientific Reports (2021)
-
Anal human papillomavirus and its associations with abnormal anal cytology among men who have sex with men
Scientific Reports (2020)
-
Human Papillomavirus awareness and vaccine acceptability among men who have sex with men from mainland China
Scientific Reports (2019)
-
HPV genotypes detected by linear array and next-generation sequencing in anal samples from HIV positive men who have sex with men in Mexico
Archives of Virology (2018)
-
Cancer risk factors among people living with HIV/AIDS in China: a systematic review and meta-analysis
Scientific Reports (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.